Nursing Informatics: Batch 2
ICT in Practice, Patient Education, and Research
Test your knowledge with these 30 questions.
Nursing Informatics: Batch 2
Question 1/30
Assessment Complete!
Here are your results, .
Your Score
27/30
90%
Test your knowledge with these 30 questions.
Question 1/30
Here are your results, .
Your Score
27/30
90%
Test your knowledge with these 30 questions.
Question 1/30
Here are your results, .
Your Score
27/30
90%
Upon completion of this module, students will be able to:
Communication in nursing is far more than the simple exchange of words; it is a dynamic, two-way process involving verbal and non-verbal cues, active listening, and the establishment of a genuine human connection. It serves as the bedrock upon which all safe and effective nursing care is built.
Counseling in nursing is a purposeful, patient-centered interaction designed to empower individuals to manage their health more effectively. It is a focused and goal-oriented process that helps patients:
Nursing communication exists on a continuum, ranging from simple social exchanges to profound therapeutic engagement. A skilled nurse can fluidly move along this continuum based on the patient's needs and the clinical context.
Description: The polite, superficial, and conventional interaction used to initiate contact and build rapport. It follows common social norms and helps put patients at ease. Examples include greeting a patient by name and making brief, non-health-related small talk.
Caution: While essential for rapport, nurses must maintain professional boundaries and avoid oversharing personal information.
Description: The factual, task-oriented communication that forms the backbone of clinical data exchange. It must be clear, direct, and accurate. Examples include asking about pain on a scale of 0-10, giving a shift report, providing patient education, or using SBAR to communicate with a physician.
Description: A patient-centered, goal-directed form of communication where the nurse helps the patient express feelings, explore problems, and find solutions. Examples include using open-ended questions ("Tell me more about..."), reflecting feelings, and using silence effectively.
Description: The deepest level where the nurse's self-awareness, authenticity, and profound empathy form the foundation of the relationship. The nurse consciously uses their genuine personality and presence as a therapeutic tool. Examples include sitting in silence with a grieving family or sharing a brief, appropriate personal insight to normalize a patient's fear.
Nurses employ various counseling styles depending on the patient's needs and the situation.
Focus: Providing clear, accurate, and understandable information. The nurse's role is a teacher, using skills like the teach-back method and simple language.
Example: Counseling a new mother on breastfeeding benefits and techniques, then asking, "Can you tell me in your own words what you will be looking for?"
Focus: A collaborative style to explore and resolve a patient's ambivalence about behavior change. The nurse's role is a guide, not a lecturer.
Example: For a patient not taking hypertension medication, asking, "What are some of the things that get in the way of taking your medicine every day?"
Focus: Providing immediate, short-term psychological first aid during an acute crisis. The nurse's role is a stabilizer and safety net.
Example: Supporting a family in the ED after an unexpected death by providing a private space and connecting them with a chaplain.
Focus: Providing emotional validation, empathy, and encouragement. The nurse's role is an empathizer and source of reassurance.
Example: Sitting with an anxious pre-op patient and saying, "It is completely normal to feel nervous right now. We are all here for you."
Focus: Assisting patients in weighing the benefits and risks of treatment options to make informed decisions. The nurse's role is an advocate and information clarifier.
Example: Helping a family understand the implications of choosing palliative care versus aggressive chemotherapy.
Focus: A structured, quick technique to help patients create a specific, achievable plan (a SMART goal) for a health behavior change. The nurse's role is a coach.
Example: Helping a patient with hypertension plan to walk for 15 minutes, three days a week, and writing the plan down together.
This table provides a quick reference for the different levels of communication and types of counseling discussed, highlighting their primary focus, the nurse's associated role, and a key example for each.
| Level/Type | Primary Focus | Nurse's Role | Key Example |
|---|---|---|---|
| Social Communication | Building Rapport | Friendly Professional | Greeting a patient |
| Informational Comm. | Exchanging Facts | Educator / Coordinator | Teaching about a new medication |
| Therapeutic Comm. | Exploring Feelings | Helper / Facilitator | Reflecting a patient's fear |
| Therapeutic Use of Self | Deep Healing Connection | Authentic Partner | Sitting in silence with the grieving |
| Health Education | Knowledge Transfer | Teacher | Diabetes self-management |
| Motivational Interviewing | Intrinsic Motivation | Guide | Exploring ambivalence to quit smoking |
| Crisis Intervention | Immediate Stabilization | Stabilizer | Supporting a family after a loss |
| Supportive Counseling | Emotional Validation | Empathizer | Easing pre-operative anxiety |
| Decision-Making | Informed Choice | Advocate | Explaining treatment options |
Effective nursing communication and counseling are not merely intuitive acts; they are grounded in well-established theoretical frameworks that provide structure, depth, and intentionality to every interaction. By understanding these foundational theories, nurses can move beyond simply 'talking to' patients to truly 'communicating with' and 'counseling' them in a purposeful and impactful manner.
This foundational theory revolutionized nursing by positioning the nurse-patient relationship as the very core of nursing practice. Peplau asserted that nursing is a dynamic, evolving partnership that unfolds in distinct, yet often overlapping, phases. Peplau's work emphasizes that the nurse's role is not simply to do things to a patient, but to work with them through a therapeutic relationship.
Description: This initial phase begins when the patient expresses a felt need. The nurse's primary task is to help the patient clarify their problem, understand expectations, and begin to establish trust. Both parties are strangers, and mutual acceptance begins here.
Scenario: Mr. Musoke, 45, is admitted with an acute exacerbation of heart failure, presenting with severe shortness of breath and anxiety.
Application: The nurse, Suubi, calmly introduces herself: "Good morning, Mr. Musoke. I'm Suubi, your registered nurse today. I'm here to help manage your breathing difficulties and ensure you're as comfortable as possible." By clearly stating her role and inviting questions, Suubi initiates the relationship, establishes professional boundaries, and begins to build foundational trust.
Description: The patient begins to identify with the nurse, seeing them as a trusted, knowledgeable helper. The patient's initial feelings of helplessness diminish as they recognize the nurse's capacity for empathy and competent care. The nurse helps the patient explore their feelings, leading to a deeper connection.
Example: A patient with newly diagnosed diabetes feels overwhelmed. As the nurse consistently listens to her fears, the patient begins to feel the nurse genuinely understands her struggle, identifying the nurse as someone who can truly help her navigate this challenge.
Description: This is the core "working" phase where the patient makes full use of the nurse's expertise to work actively toward their health goals. The patient takes an active role in problem-solving, and the nurse acts as a resource person, counselor, and teacher.
Scenario (Combining Identification & Exploitation): Mrs. Nalwanga, 55, with newly diagnosed Type 2 Diabetes, is struggling with dietary changes. She says, "Nurse, I just can't give up my g-nut paste sauce and matooke!"
Application: The nurse responds empathetically: "Mrs. Nalwanga, it sounds like you're finding it incredibly hard to adjust... Let's work together to identify some realistic swaps or portion adjustments you'd be comfortable with." By acknowledging her cultural context and shifting to collaborative problem-solving, the nurse enables Mrs. Nalwanga to feel understood (Identification) and actively engage in finding solutions (Exploitation).
Description: The formal conclusion of the therapeutic relationship as the patient's needs are met and they regain independence. It is a planned termination where progress is reviewed and gains are consolidated.
Scenario: Mr. Kato, 70, is preparing for discharge after a successful prostatectomy.
Application: On the day of discharge, the nurse asks Mr. Kato to demonstrate his wound care one last time and explain his medication schedule. "Excellent, Mr. Kato! You're ready. Remember, if you have any questions... please don't hesitate to call." This reinforces the patient's autonomy, validates his progress, and formally concludes the in-hospital relationship while providing a pathway for future support.
Carl Rogers' highly influential humanistic theory revolutionized counseling and profoundly impacted nursing communication. The core belief is that individuals possess an inherent drive to fulfill their potential, and the nurse's role is to create a supportive emotional environment that allows the patient to access this inner wisdom and solve their own problems. This is achieved through three core conditions that facilitate therapeutic change:
Description: Accepting and respecting the patient as a person of inherent worth and dignity, without judgment, regardless of their choices or behaviors. It means valuing the patient as a unique individual and conveying a non-evaluative stance to foster psychological safety.
Scenario: Mr. Kamya, a 60-year-old with severe COPD, continues to smoke despite repeated education.
Application: Instead of showing frustration, the nurse employs UPR: "Mr. Kamya, I understand that quitting smoking is incredibly difficult... My concern is for your health, and I want to support you. Let's talk about what makes it so hard for you right now, without any pressure." This non-judgmental approach keeps the door open for an honest conversation, allowing Mr. Kamya to feel safe enough to discuss his barriers without fear of condemnation.
Description: The ability to accurately sense the patient's private world and feelings as if they were your own, but without losing the "as if" quality. It involves deep listening and reflecting back the patient's feelings to validate their emotional experience.
Scenario: Ms. Kyakuwa, 30, expresses overwhelming fear and despair after a new diagnosis of advanced metastatic cancer.
Application: The nurse responds with genuine concern, reflecting the depth of the patient's experience: "Ms. Kyakuwa, it sounds like receiving this news has been terrifying and incredibly overwhelming. It's a massive shock, and it must feel like your world has been turned upside down... those feelings are completely understandable." This makes her feel profoundly heard and validated.
Description: The nurse being authentic, transparent, and self-aware within the relationship, rather than hiding behind a professional façade. It involves aligning one's inner feelings and outer expressions to foster profound trust through authenticity.
Scenario: A young, anxious patient, Sarah, asks her nurse, "Would you be scared if this were your surgery? Are you sure everything will be okay?"
Application: Rather than giving a hollow reassurance, a congruent nurse might respond honestly: "Sarah, it's completely normal to feel scared... While I can't know exactly how you feel... I can tell you that facing surgery is a big event, and it's natural to have those worries. My role is to make sure you have all the information you need... and to support you through every step. We will be right here with you." This authentic response builds profound trust.
Motivational Interviewing is a powerful, evidence-based counseling method that is particularly effective for addressing the common challenge of ambivalence—the state of having mixed feelings about changing a health behavior. It represents a profound shift from the traditional, expert-led model to a collaborative, guiding partnership. MI acknowledges that forcing change often leads to resistance, whereas supporting a patient's autonomy and internal motivation makes lasting change far more likely.
The fundamental premise of MI is that people are inherently ambivalent about change. The nurse's role is not to confront or persuade, but to become a collaborative partner who skillfully explores this ambivalence, listening intently and helping the patient elicit and strengthen their own reasons for change. Motivation must come from within.
The practice of MI is guided by a specific mindset or "spirit":
OARS is a mnemonic for the core communication skills used in MI. These micro-skills are foundational for building rapport and facilitating "change talk."
These are questions that cannot be answered with a simple "yes" or "no." They are invitations for the patient to tell their story and explore their thoughts and feelings in depth.
Examples:
These are genuine statements that recognize and reinforce the patient's strengths, abilities, efforts, and good intentions, no matter how small. Affirmations are crucial for building confidence (self-efficacy).
Examples:
Arguably the most critical skill in MI, this involves listening to what the patient says and reflecting back the meaning or essence of their message in the nurse's own words. It validates the patient's experience and confirms understanding.
Types of Reflections:
Summaries are a collection of reflections that pull together the patient's statements, especially their "change talk." This demonstrates that the nurse has been listening and reinforces the patient's own motivation by allowing them to hear their arguments for change.
Example:
"So let me see if I have this right... You've been feeling concerned about your energy levels and how your weight affects your ability to play with your grandchildren... you think starting with a daily 15-minute walk is something you could realistically do... Is that a fair summary?"
The practical application of MI skillfully integrates the OARS skills with the spirit of MI to guide conversations towards positive health changes.
Description: "Change talk" is any statement from the patient that expresses a desire, ability, reason, need, or commitment to change. The goal of MI is to create an environment where the patient, not the nurse, voices the arguments for change.
Scenario: A patient with obesity, Mr. Mutebi, is at risk for diabetes and feels overwhelmed by the idea of weight loss.
Application: The nurse uses open-ended questions: "What concerns, if any, do you have about your current weight?" or "If you were to lose a small amount of weight, what do you imagine some of the good things might be?"
Why it's powerful: This is more effective than the nurse listing generic reasons. When the patient voices the benefits themselves, their internal motivation is strengthened, and they take psychological ownership of the reasons for change. It becomes their idea, not a directive.
Description: Resistance, or "sustain talk" (arguments for staying the same), is a normal part of the process. The nurse does not confront or argue with resistance but "rolls with it," acknowledging the patient's perspective to de-escalate defensiveness and keep the conversation collaborative.
Scenario: A patient, Ms. Nansamba, states, "I know I should exercise, but I just never have the time."
MI Application: The nurse uses a complex reflection: "So, time is a really significant factor for you right now... It sounds like your schedule is already completely full and finding an extra moment feels impossible. Given that, I wonder if we could just brainstorm for a minute about where even 10-15 minutes of movement might fit in?"
Why it's powerful: By not arguing, the nurse maintains a collaborative relationship. Validating the patient's feeling reduces defensiveness and keeps the conversation open. The nurse then invites the patient into a problem-solving partnership, empowering them to generate their own solutions.
Description: A simple tool to assess a patient's perceived importance of and confidence in making a change. It uses scaling questions (0-10) to elicit "change talk" and explore ambivalence.
Scenario: Discussing smoking cessation with a patient, Mr. Lugolobi.
Application: The nurse asks, "On a scale from 0 to 10, where 0 is 'not important at all' and 10 is 'extremely important,' how important is it for you to quit smoking right now?" The patient says, "A 4." The crucial MI follow-up is not "Why so low?" but rather: "That's helpful, thank you. Can I ask, why did you say a 4 and not a 2 or a 3?"
Why it's powerful: This question cleverly prompts the patient to articulate their own arguments for change. They have to explain what makes them a "4"—what positive motivations they already possess (e.g., "Well, I know it's bad for my breathing, and my grandchildren have been asking me to stop..."). This elicits internal "change talk" directly from the patient, reinforcing their own motivation.
Upon completion of this module, students will be able to:
Expanded Definition: Online communication is the process of creating and sharing meaning through digital or internet-based platforms. This process involves both asynchronous communication (where there is a time lag, like email) and synchronous communication (which happens in real-time, like a video call).
The Central Challenge: The Absence of Cues. In face-to-face communication, we rely heavily on non-verbal cues (body language, facial expressions, tone of voice). In the online environment, these are often absent, meaning the words we type and digital cues (emojis, punctuation, capitalization) carry enormous weight and can be easily misinterpreted.
| Benefit | Expanded Explanation and Ugandan Context Example |
|---|---|
| 1. Accessibility & Flexibility | Students and faculty can communicate from anywhere. Invaluable for a student on a rural placement who can still access lecture notes on Moodle. |
| 2. Wider Reach | Digital platforms collapse distance. A specialist in Kampala can provide a telehealth consultation to a nurse and patient in a remote health center. |
| 3. Faster Information Sharing | Urgent updates can be disseminated instantly. A course leader can email all students about a room change, or a WhatsApp group can quickly coordinate tasks. |
| 4. Development of Digital Literacy | Builds essential ICT competencies. Skills in using an LMS or participating in video calls are directly transferable to using EHRs in a hospital. |
| 5. Support for Blended Learning | Online tools supplement face-to-face instruction. A lecturer can post a video to watch before class, freeing up in-person time for interactive case studies. |
| 6. Inclusive Participation | Can be a more comfortable space for shy students to express themselves in a discussion forum without the pressure of speaking up in a large lecture hall. |
| 7. Permanent Record Keeping | Digital communication creates a verifiable record. A student can revisit written feedback, and important announcements can be accessed at any time. |
| What Could Go Wrong | Consequences and How to Avoid It |
|---|---|
| 1. Lack of Clarity or Misunderstanding | A short, direct message can be perceived as rude. Avoid by: Using polite language and providing constructive, specific feedback. |
| 2. Delayed Response Time | Significant delays can slow workflows or cause missed deadlines. Avoid by: Setting clear expectations for response times (e.g., "I will respond within 48 hours"). |
| 3. Unprofessional Language or Tone | Using slang, informal abbreviations, or inappropriate emojis damages your professional reputation. Avoid by: Always maintaining a professional tone. NEVER USE ALL CAPS. |
| 4. Privacy and Confidentiality Violations | Sharing patient-identifying information on insecure platforms is a serious breach with legal and professional repercussions. Avoid by: Never discussing patient details on non-secure platforms. |
| 5. Exclusion of Students (The Digital Divide) | Not all students have reliable and affordable internet or suitable devices. Avoid by: Educators should be mindful and provide alternative ways to access materials (e.g., downloadable resources). |
| 6. Cyberbullying or Disrespect | Posting disrespectful comments creates a toxic learning environment. Avoid by: Adhering strictly to professional respect. Report any instances of cyberbullying to faculty immediately. |
"Netiquette" (Network Etiquette) is the code of conduct for respectful and effective online communication.
Write in short, clear sentences. Use a descriptive subject line in emails and always proofread before sending.
Always use a proper salutation and closing. Avoid sarcasm and never type in all caps, as it is perceived as shouting.
Acknowledge receipt of important messages, even if you need more time to provide a full response.
This is the most important rule. Do not share any personal or patient details in non-secure environments.
Remember that humor, idioms, and context may vary. Strive for clear, universally understood language.
Professional ethics do not disappear online; they are simply applied in a new context.
| Ethical Principle | Description & Example |
|---|---|
| 1. Confidentiality | Protecting private information. Ex: A nurse avoids posting any detail of a patient's condition in online forums or WhatsApp groups. |
| 2. Privacy | Respecting personal boundaries. Ex: Ensuring telehealth consultations are held in a private, secure environment where others cannot overhear. |
| 3. Professionalism | Maintaining appropriate tone and conduct. Ex: Using polite, clear, and respectful language in emails with students, patients, and colleagues. |
| 4. Informed Consent | Ensuring agreement before sharing information. Ex: Obtaining explicit written consent from all students before posting photos of a training session online. |
| 5. Accountability | Taking responsibility for one's digital actions. Ex: A nurse acknowledges and promptly corrects an error made in an online report. |
| 6. Integrity and Honesty | Being truthful and transparent. Ex: A nursing student ensures all online assignments are original and properly referenced. |
| 7. Respect and Courtesy | Treating others with dignity. Ex: In an online debate, a student provides counterarguments based on evidence, not personal attacks. |
| 8. Non-maleficence | Ensuring communication does not cause harm. Ex: Actively avoiding cyberbullying, gossip, or spreading misinformation. |
| 9. Justice and Fairness | Ensuring equitable treatment and access. Ex: An educator ensures all students have equal access to online materials, being mindful of the digital divide. |
| 10. Data Protection and Security | Safeguarding electronic records. Ex: Using secure, password-protected hospital portals for patient updates, never personal email or insecure messaging apps. |
Use professional email addresses for all official communication, not personal accounts (e.g., your.name@university.ac.ug, not coolnurse25@gmail.com).
Pause before you post. Avoid sending messages when you are emotionally upset or angry. Step away and come back later with a clear mind.
Be a steward of truth. Verify the authenticity of health-related information before sharing it online. Do not contribute to the spread of misinformation.
Know the rules. Adhere to the ICT and social media policies of your institution and the professional code of conduct of the Uganda Nurses and Midwives Council.
Maintain strict digital boundaries. Do not "friend" or follow patients on personal social media accounts. Keep your professional and personal online identities separate.
A quiz on Communication and Counseling in Nursing.
1. What is considered the "cornerstone of all patient care" according to the text?
Correct (b): The text explicitly states that Communication is the "Cornerstone of all patient care."
2. What is a primary purpose of counseling in nursing?
Correct (b): Counseling is a goal-oriented process designed to help patients cope with their situations, understand their health, and make informed decisions.
3. When a nurse greets a patient and makes small talk, what level of communication is this?
Correct (d): Level 1, Social Communication, is the superficial, polite interaction used to build rapport and put patients at ease, such as a simple greeting.
4. A nurse providing patient education, such as "This is how you use your new inhaler," is engaging in what level of communication?
Correct (b): Level 2, Structured / Informational Communication, is factual, task-oriented, and includes providing specific patient education and instructions.
5. When a nurse reflects a patient's feelings by saying, "It sounds like you're feeling very overwhelmed," what level of communication is this?
Correct (c): Level 3, Therapeutic / Helping Communication, focuses on exploring the patient's emotions and problems, often by using techniques like reflecting feelings.
6. The deepest level of communication, based on the nurse's self-awareness, authenticity, and empathy, is known as what?
Correct (d): Level 4, Therapeutic Use of Self, is the highest and deepest level, where the nurse's personal attributes form the foundation of the healing relationship.
7. Counseling a newly diagnosed diabetic on blood glucose monitoring falls under which type?
Correct (c): This involves providing factual information and teaching essential skills, which is the core of Health Education and Informational Counseling.
8. Which type of counseling helps a patient explore ambivalence about quitting smoking and identify their own reasons for change?
Correct (b): Motivational Interviewing (MI) is specifically designed to explore a patient's ambivalence and elicit their own intrinsic motivation for behavior change.
9. Providing immediate, short-term support to individuals in an acute emotional crisis is the focus of which type of counseling?
Correct (c): Crisis Intervention Counseling is focused on providing immediate, short-term psychological first aid to help someone navigate an acute crisis.
10. Helping a patient and family understand the choice between hospice and chemotherapy is what type of counseling?
Correct (c): Decision-Making Counseling involves helping patients weigh the benefits, risks, and implications of different treatment options to make an informed choice.
11. Hildegard Peplau's Theory of Interpersonal Relations describes a process with how many overlapping phases?
Correct (c): Peplau's influential theory describes the nurse-patient relationship as a process with four distinct but overlapping phases: Orientation, Identification, Exploitation, and Resolution.
12. In Peplau's theory, the phase where the patient fully uses the nurse's services to address their needs is called what?
Correct (c): The "Exploitation" phase is the working phase where the patient actively engages with and utilizes the resources and services offered by the nurse to meet their health goals.
13. Carl Rogers' Person-Centered Therapy posits that the counselor's attitude is more important than their what?
Correct (b): Rogers' theory emphasizes that the therapeutic relationship, built on the counselor's attitude, is the primary agent of change, more so than any specific techniques or interventions.
14. What is one of the three core conditions in Carl Rogers' Person-Centered Therapy?
Correct (c): The three core conditions are Unconditional Positive Regard (acceptance), Empathic Understanding, and Congruence (genuineness).
Incorrect: The other options are contrary to the principles of Rogers' non-directive, client-centered approach.
15. Using an open-ended question like, "What concerns you about your current weight?" is an example of what MI technique?
Correct (c): "Eliciting Change Talk" involves using open-ended questions to have the patient voice their own reasons and motivations for change.
Incorrect (a): Rolling with Resistance involves not arguing with a patient's resistance.
Incorrect (b): Using the Readiness Ruler involves a numerical scale.
16. Counseling is focused and goal-oriented, helping patients to cope, understand, and make _________.
17. Level 2 communication is for assessing, informing, educating, and _________ care.
18. MI is designed to strengthen a person's own motivation and _________ to change.
19. In Peplau's theory, during the _________ phase, the patient identifies with the nurse and trust develops.
20. Carl Rogers' core condition of _________ (Genuineness) means being authentic and transparent.
Your Score:
0%
0 / 0 correct
Nursing documentation is the systematic, accurate, and comprehensive recording of all aspects of the nursing process – from initial patient assessments and diagnoses to the planning and implementation of interventions and the evaluation of outcomes.
This encompasses both written and, increasingly, electronic formats within an Electronic Health Record (EHR) system. In contemporary healthcare, the EHR is the primary, legally binding repository for nursing documentation.
While often perceived as a legal safeguard, accurate and thorough nursing documentation is the bedrock of professional nursing practice and the engine driving modern healthcare.
It is irrefutable proof that care was delivered. In legal disputes, "if it wasn't documented, it wasn't done."
Serves as the primary communication conduit among the multidisciplinary team, ensuring seamless care transitions.
Demonstrates the nurse's clinical judgment, decision-making, and professional accountability for their actions.
Justifies the services rendered, which is essential for accurate billing and impacts the financial sustainability of health institutions.
Patient records are audited to ensure compliance with standards, identify deviations, and pinpoint areas for systemic improvement.
Aggregated, de-identified nursing data from EHRs is an invaluable asset for research, helping to evaluate interventions and develop new evidence-based practices.
A nursing language, or standardized nursing terminology, is a structured vocabulary specifically developed by nurses for nurses.
Its purpose is to accurately describe, communicate, and quantify the unique contributions of nursing practice – patient problems (diagnoses), interventions, and outcomes.
Focus: Clinical judgments about patient responses to health problems. It helps nurses systematically identify and articulate problems within the nursing scope.
Example: Acute Pain related to surgical incision as evidenced by patient verbalizing pain score of 8/10.
Focus: A comprehensive classification of treatments that nurses perform. It provides a clear, consistent way to describe what nurses do.
Example: Pain Management, with activities like "Administer prescribed analgesia" and "Provide non-pharmacological comfort measures."
Focus: A standardized classification of patient states or behaviors that are influenced by nursing interventions. It allows nurses to objectively measure the effectiveness of their care.
Example: Pain Level, with indicators like "Patient reports pain score less than 3/10."
Focus: A comprehensive practice and documentation standard for community, public health, and home care settings. It is highly valuable in the Ugandan context for community health nurses and VHTs.
Focus: A unified, global nursing terminology developed by the ICN to represent nursing practice worldwide. It promotes data interoperability and strengthens nursing's voice on the global stage.
Nurses are the largest and most consistent generators of patient data. They are at the bedside 24/7, and their constant interaction yields a wealth of information that, when systematically documented, forms the holistic narrative of a patient's health journey.
Content: Name, age, sex, contact details, next of kin, and unique identifiers. In Uganda, this may include tribe and district of origin for cultural context and public health tracking.
Relevance: Crucial for accurate patient identification, contextualizing care, and forming the foundational layer for all other health data.
Content: Blood pressure, temperature, pulse, respiratory rate, oxygen saturation, and pain level.
Relevance: Provide immediate, critical insights into a patient's physiological status. Trends in vital signs are primary triggers for nursing interventions.
Content: Detailed evaluations of all body systems, including pain, wound, neurological, nutritional, respiratory, and psychosocial assessments.
Relevance: Form the basis for nursing diagnoses, provide a baseline for evaluating changes, and guide the development of individualized care plans.
Content: All actions performed by the nurse, including medication administration, patient and family education, wound care, therapeutic communication, monitoring, and ADL assistance.
Relevance: Demonstrates the direct impact of nursing care and provides data for evaluating the effectiveness of specific interventions.
Content: The patient's measurable response to nursing interventions, including improvement in symptoms, functional gains, stabilization, and discharge readiness.
Relevance: Essential for evaluating the effectiveness of the care plan, modifying interventions, and demonstrating the value of nursing care.
Nursing is a dynamic profession with a distinct set of attributes. Understanding these characteristics is crucial to appreciating the profound impact of nursing informatics on professional practice.
Historically, health information systems have been effective at capturing managerial and dependent activities. However, the crucial independent work of nurses—the clinical observations, critical thinking, patient education, and compassionate care—has too often been buried in unstructured narrative notes, remaining largely "invisible" within healthcare data systems.
For decades, the profound impact of nursing care was difficult to quantify. Research has consistently shown that the quality and quantity of nursing care directly influence critical patient outcomes, with many adverse events linked to inadequate nursing vigilance:
The widespread adoption of EHRs represents a transformative shift. By moving beyond free-text narrative, EHRs allow for the capture of nursing data in a structured, analyzable format.
Instead of subjective notes, EHRs employ dropdown menus, checkboxes, templated flowsheets, and standardized terminologies (NANDA-I, NIC, NOC). This is the critical step that transforms narrative into discrete, machine-readable data.
Structured data can be easily aggregated, queried, and analyzed. This allows researchers and administrators to identify patterns and correlate nursing activities with patient outcomes.
This newfound visibility is critical. With data-driven evidence, administrators can now see, with undeniable clarity, how factors like nurse staffing levels and specific nursing interventions directly impact patient safety, satisfaction, and efficiency.
In nursing informatics, a standard is a formal agreement that specifies precise criteria, definitions, or formats to be used consistently across different systems. In healthcare, standards are essential for safe, effective, and interoperable communication and data exchange.
The American Nurses Association endorses and advocates for standardized nursing terminologies.
The International Council of Nurses develops and promotes the global ICNP terminology.
The National League for Nursing focuses on integrating informatics into nursing education.
Health Level Seven International creates standards for exchanging electronic health information.
The International Organization for Standardization sets global standards for healthcare informatics.
Ensures all providers understand each other precisely, reducing ambiguity. A coded diagnosis means the same thing in Kampala as it does in London.
Allows nursing data to be consistently collected and compared across different hospitals, regions, and countries for large-scale research.
Allows administrators to accurately plan for staffing, equipment, and budgets based on standardized data, not just anecdotes.
Structured, standardized data is the fuel for CDSS, which can trigger alerts, suggest interventions, and provide guidelines to enhance patient safety.
The financial value of nursing care remains obscure, leading to underfunding and an inability to bill for nursing contributions effectively.
Decisions about staffing and training are made without objective data, often resulting in suboptimal resource allocation and increased workload.
The true impact of nursing on patient outcomes cannot be calculated, perpetuating the invisibility of nursing's value.
Different facilities cannot easily exchange or understand each other's nursing data, creating silos of information and impeding coordinated care.
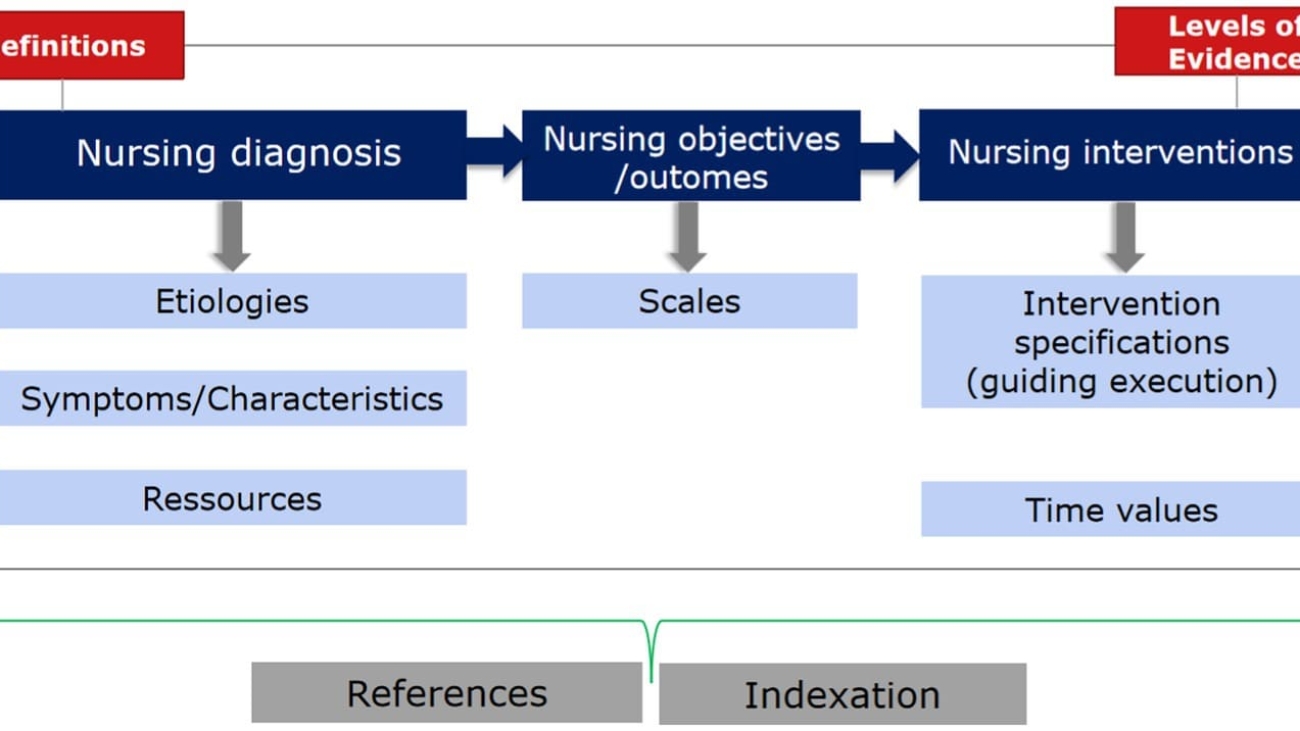
These three terminologies represent the core of the nursing process (Diagnosis, Intervention, Outcome). When used together, they create a complete, coded plan of care.
A global, combinatorial standard from the ICN. Its design allows local nursing practices, like those in Uganda, to be represented in a globally understood format, facilitating international collaboration.
The most comprehensive clinical terminology in the world. Nursing concepts can be mapped to SNOMED CT, ensuring nursing data is interoperable with all other clinical data in a comprehensive EHR.
A standard used to identify laboratory observations and clinical measurements. It provides universal codes for data like vital signs, ensuring that measurement data collected by nurses can be unambiguously understood and exchanged.
Consider a patient with malaria. Using standardized language in an EHR creates a clear, concise, and universally understood record:
This structured documentation ensures every provider on the team instantly understands the patient's problem, plan of care, and expected trajectory.
The journey towards standardized nursing documentation has been a long and evolutionary process, moving from rudimentary, often subjective records to sophisticated, interoperable digital systems.
Long before the term "informatics" existed, Nightingale systematically collected and analyzed patient statistics during the Crimean War. She used data visualization (e.g., her famous "Coxcomb" charts) to prove that nursing interventions like improved sanitation directly saved lives, providing the first scientific evidence of nursing's impact on patient outcomes.
To effectively manage health information, it's essential to understand its fundamental components.
The NMDS is a globally recognized, standardized set of essential data elements collected for every patient receiving nursing care. It includes nursing care elements (diagnosis, intervention, outcome), patient demographics, and service elements (admission/discharge dates). Its purpose is to provide a consistent framework for aggregating nursing data for research, policy, and resource allocation.
Nurses in antenatal, postnatal, and immunization programs collect specific data elements for every mother and child. These elements include: Number of ANC Visits, Parity, Gravidity, Delivery Outcome, Child's Immunization Status, Weight at Birth, and HIV Status of Mother.
Significance: This aggregated data set, often entered into platforms like DHIS2, contributes to vital public health reports like the Uganda Demographic and Health Surveys (UDHS). The UDHS informs national health policy, program planning, and resource allocation. Without the diligent collection of these standardized data elements by nurses, evidence-based policy decisions in Uganda would be impossible.
A robust nursing language must have several key characteristics to be effective.
| Characteristic | Ugandan Context Example |
|---|---|
| 1. Parsimony | Uses the fewest words possible. Instead of "the surgical wound is not healing well and has pus coming out," a nurse uses: "Impaired Skin Integrity." |
| 2. Comprehensiveness | Covers all aspects of care. For an HIV patient, a nurse documents: “Ineffective Health Management,” “Risk for Infection,” and “Spiritual Distress.” |
| 3. Mutual Exclusivity | Each diagnosis refers to a unique problem. “Risk for Infection” is distinct from “Risk for Ineffective Coping.” |
| 4. Unambiguity | Each term has one clear meaning. “Acute Pain” (post-C-section) is different from “Chronic Pain” (persistent low back pain). |
| 5. Leveling (Hierarchy) | Structured from general to specific. A general diagnosis of “Impaired Mobility” can be specified as “Impaired Bed Mobility.” |
| 6. Codifiability | Can be coded for use in EHRs and national systems like DHIS2, allowing for national tracking of hospital-acquired infections. |
| 7. Universality | Applicable across all settings. “Ineffective Breastfeeding” can be used in a neonatal ICU, a rural clinic, or a home visit. |
| 8. Reflects Nursing Practice | Focuses on human responses. Instead of only documenting “Malaria,” the nurse documents: “Hyperthermia,” “Risk for Fluid Volume Deficit,” and “Activity Intolerance.” |
| 9. Flexibility | Can be updated for new health needs. The diagnosis “Risk for Infection” is flexible enough to be applied to new health threats. |
| 10. Evidence-Based | Supported by research. Using diagnoses like “Fatigue,” “Anxiety,” and “Risk for Infection” for chemotherapy patients is based on global oncology nursing evidence. |
Nursing Diagnosis (NANDA-I): Hyperthermia related to infectious process as evidenced by a body temperature of 39.5°C, flushed skin, and tachycardia.
NIC (Interventions):
NOC (Outcomes):
Nursing Diagnosis (NANDA-I): Impaired Skin Integrity related to surgical incision as evidenced by redness and swelling around the wound edges.
NIC (Interventions):
NOC (Outcomes):
Nursing Diagnosis (NANDA-I): Ineffective Health Management related to knowledge deficit about ART regimen as evidenced by multiple missed clinic appointments and a detectable viral load.
NIC (Interventions):
NOC (Outcomes):
A quiz on Documentation and the Nursing Language.
1. What is the definition of "Nursing documentation" according to the text?
Correct (b): The text directly defines "Nursing documentation" as "the written or electronic record of nursing assessments, interventions, and outcomes."
2. Which of the following is NOT listed as an importance of nursing documentation?
Correct (b): The "Importance" section lists Evidence of care, Continuity, Accountability, Billing, Auditing, and Research. Staff social events are not related to documentation.
3. The terminology and vocabulary used by nurses to describe, communicate, and document their practice is known as what?
Correct (b): The text defines "Nursing language" as the specific terminology and vocabulary used by nurses in their practice.
4. Which of the following is an example of "patient demographics" data?
Correct (c): Patient demographics include data like age, sex, and contact information.
Incorrect: Blood pressure is a vital sign, pain score is a clinical assessment, and drug administration is an intervention.
5. According to the text, which type of nursing activities are often NOT captured by most information systems?
Correct (c): The text states that while managerial and dependent activities are often captured, the independent, autonomous activities of nursing are frequently not.
6. The absence of nursing data makes nursing invisible and often leads to what kind of outcomes being associated with nursing?
Correct (c): When nursing's contribution isn't visible in the data, nursing is often measured by negative outcomes like infections, pressure sores, and falls.
7. How do EHRs increase the visibility of nursing data?
Correct (c): EHRs increase data visibility by storing it in structured, retrievable fields that can be analyzed for research, quality improvement, and demonstrating nursing's impact.
8. What is a "standard" in the context of standardized terminology?
Correct (b): A standard is a formal, documented agreement containing precise criteria and definitions that must be used consistently to ensure clarity and interoperability.
9. Which organization is listed as responsible for creating standards in healthcare documentation?
Correct (c): The text explicitly lists the ANA, ICN, and NLN as organizations responsible for creating standards.
10. What is a disadvantage of NOT documenting with standardized language?
Correct (c): Without standardized, machine-readable data, it is very difficult to build the rules and logic required for effective clinical decision support systems.
Incorrect: The other options are the opposite of what happens; without standardized data, funding, calculating contributions, and planning resources all become more difficult.
11. In standardizing terminologies, what is the second task after identifying data elements?
Correct (b): The process involves 1. Identifying data elements, 2. Developing the terminology, and 3. Classifying the terminology.
12. What does NANDA-I primarily describe in standardized nursing language?
Correct (b): NANDA-I is the standardized terminology for nursing diagnoses, such as 'Impaired Skin Integrity'.
Incorrect: NIC describes interventions, and NOC describes outcomes.
13. Which characteristic ensures that each term has one clear meaning (e.g., "Acute Pain" vs. "Chronic Pain")?
Correct (c): "Unambiguity" is the characteristic that ensures each term has one clear, distinct meaning to avoid confusion.
14. When a nurse documents "Hyperthermia" for a malaria patient, this exemplifies which characteristic of nursing language?
Correct (c): This demonstrates "Reflects Nursing Practice" because it focuses on the patient's response and the nursing-relevant problem (Hyperthermia) rather than just the medical diagnosis (Malaria).
15. The Uganda Maternal and Child Health Data Set, where nurses enter ANC visits, parity, etc., is an example of what?
Correct (b): A Data Set is a structured collection of related data elements, such as the various pieces of information collected during a maternal health visit.
Incorrect (a): A data element is a single unit, like "Parity = 2."
16. Nursing language terminology includes NIC, NOC, NANDA-I, and _________.
17. One of the characteristics that defines nursing as a profession is having a defined _________.
18. Studies have shown that the more registered nurses there are, the fewer the _________ outcomes.
19. A standard is a documented agreement with precise criteria that must be used _________.
20. The characteristic of nursing language called _________ means it can be coded for use in EHRs.
Your Score:
0%
0 / 0 correct
Upon successful completion of this module, students will be able to:
ICT in health and nursing care involves using digital tools to improve the efficiency, accuracy, and accessibility of clinical information, ultimately enhancing patient care. These technologies are used in various areas, such as electronic health records (EHRs), remote monitoring, and telemedicine.
While ICT offers significant benefits like reducing geographic barriers and enabling better communication, challenges persist regarding implementation, training, and potential depersonalization of care.
Nursing informatics in client education is the strategic and purposeful application of ICT to design, deliver, and manage educational interventions for patients, their families, and caregivers. It moves far beyond simply handing out a leaflet or giving verbal instructions. Instead, it leverages digital tools to create dynamic, interactive, and personalized learning experiences tailored to individual needs and cultural contexts.
The core objective is to significantly improve health literacy – the degree to which individuals can obtain, process, and understand basic health information to make appropriate health decisions. By integrating informatics, nurses can:
The integration of Information and Communication Technologies (ICT) into healthcare delivery offers a powerful set of tools to improve care, but it also presents significant challenges that must be carefully managed.
| Advantages | Disadvantages |
|---|---|
|
|
Nurses have always been at the forefront of patient education. With the advent of ICT, their role has become even more central, sophisticated, and impactful. By leveraging informatics tools, nurses can transform how they educate, leading to more effective and sustainable patient outcomes.
Instead of just telling a patient how to use an inhaler, a nurse can use an animated video on a tablet to visually demonstrate the technique. This enhances comprehension, especially for complex procedures or visual learners.
ICT platforms ensure all patients receive consistent, up-to-date information that aligns with current clinical guidelines. This reduces variations in care and minimizes misinformation.
Mobile technology and telehealth allow nurses to connect with patients remotely, providing education and support where it is most convenient. This is vital for patients in rural or underserved areas with transportation barriers.
For chronic conditions like diabetes, hypertension, and HIV, nurses can use ICT to deliver personalized reminders, educational modules, and monitor patient-reported outcomes, enabling continuous support outside of clinic visits.
Informatics tools can help nurses track patient engagement with educational materials (e.g., through quizzes or feedback) and adapt their teaching strategies accordingly, allowing for a more personalized and effective approach.
We explore specific ICT methodologies that nurses are using or can effectively use in Uganda to deliver impactful client education.
This methodology leverages rich sensory input—videos, animations, interactive graphics, and audio clips—to explain complex health topics. It's particularly effective for individuals with varying literacy levels, diverse language backgrounds, or for illustrating intricate procedures. The visual and auditory components can enhance engagement and memory retention significantly.
mHealth harnesses the ubiquitous nature of mobile phones to deliver health information, personalized reminders, and facilitate communication. Given that over 74% of Uganda's population has access to mobile phones, mHealth presents an unparalleled channel for reaching diverse populations, especially in remote areas.
Telehealth utilizes video conferencing, audio calls, and secure messaging to facilitate remote interactions between patients and providers. This technology reduces geographical barriers, minimizes travel costs, and can improve access to specialized care, particularly in resource-limited settings.
Patient portals are secure online platforms, often integrated with the EHR, that grant patients direct access to their personal health information. These portals empower patients to view lab results, medication lists, schedule appointments, and access health education resources.
Discharge planning is not merely an administrative task performed at the end of a hospital stay; it is a critical, coordinated, and interdisciplinary process that begins upon admission and continues until the patient has successfully transitioned to their next level of care. The goal is to ensure a safe, smooth, and sustainable transition, preventing complications and reducing preventable readmissions.
Nursing informatics transforms this process from a reactive, paper-based checklist into a dynamic, proactive, and technology-enhanced system. It moves from simply telling a patient what to do to equipping them with the knowledge, tools, and ongoing support necessary for self-management. This transformation involves:
Nurses are the linchpins of effective discharge planning. By integrating informatics into their practice, nurses elevate their capacity to ensure safe and successful transitions in several key areas:
Nurses use EHRs to generate accurate, personalized medication lists, ensuring patients understand the name, purpose, dosage, schedule, side effects, administration, and proper storage of their medicines.
Nurses use electronic scheduling systems to book all necessary appointments and generate clear printouts or send SMS reminders, ensuring patients know the dates, locations, purpose, and any preparation required.
Nurses access digital guidelines, customizing them for the patient's needs and local context, discussing restrictions and recommendations using locally available and affordable foods.
Nurses use multimedia tools on tablets to visually demonstrate complex procedures like wound cleaning and dressing changes, and teach patients how to identify signs of infection.
Nurses leverage ICT to create clear, concise lists of specific symptoms that require immediate medical attention, often reinforced with patient-friendly visuals (e.g., for post-surgery or post-delivery care).
Uganda is increasingly embracing ICT in healthcare, offering inspiring examples of how informatics enhances discharge planning.
Mechanics: Nurses print discharge summaries with custom QR codes linking to videos or infographics on relevant health topics (e.g., "newborn bathing techniques" or "healthy eating for diabetics using local foods").
Impact: This empowers patients to access visual and auditory information at home, at their own pace, bridging literacy gaps and improving retention.
Mechanics: An integrated electronic system helps manage discharge medications, automates checks for drug interactions, and generates a clear, printed schedule. It also flags patients for follow-up SMS reminders for medication refills.
Impact: This significantly reduces medication errors, improves adherence, and minimizes the risk of patients running out of essential medicines.
Mechanics: Oncology nurses create and moderate secure, patient-only WhatsApp groups for patients discharged after cancer treatment.
Impact: Nurses proactively share education on managing side effects, while patients can ask questions and offer mutual support. This virtual community extends care beyond the hospital, reducing isolation and anxiety.
Mechanics: Nurses use a smartphone app to register high-risk children (e.g., from neonatal or malnutrition wards) and their caregivers. The platform then triggers personalized, stage-based SMS reminders with actionable health advice.
Impact: Research shows this program significantly changes caregiver behavior, increasing adherence to follow-up care, promoting healthy practices, and even fostering male involvement in child health.
Implementing ICT in discharge planning in Uganda brings immense benefits but also faces considerable hurdles that must be addressed for successful and equitable implementation.
An information system (IS) is a complex, integrated framework of people, processes, and technology designed to collect, process, store, and distribute data. In the Ugandan healthcare landscape, these systems are foundational to managing patient care, conducting public health surveillance, and driving health research. They are the digital backbone upon which a more data-driven health system can be built.
The cornerstone of Uganda's health data management, DHIS2 is a web-based platform used by the Ministry of Health for aggregating routine health service data from all levels of the health system.
Nursing Informatics Role: Nurses in leadership and public health roles are crucial contributors, ensuring accurate data entry for immunizations, disease incidence, etc. They use DHIS2 dashboards to monitor disease outbreaks, track health indicators, and evaluate program effectiveness, informing resource allocation and public health interventions.
An open-source Electronic Medical Record (EMR) system customized as UgandaEMR. Unlike DHIS2, it focuses on managing individual patient data for clinical care at the facility level, especially for chronic conditions like HIV/AIDS.
Nursing Informatics Role: Nurses are primary end-users, inputting patient demographics, vital signs, assessments, and medication records. They use it to track treatment adherence, monitor lab results (e.g., viral loads, CD4 counts), schedule appointments, and receive alerts, improving continuity of care.
Comprehensive, integrated systems designed to manage all administrative, financial, and clinical aspects of a hospital, including patient registration, billing, and inventory control.
Nursing Informatics Role: Nurses interact with HIS for patient admission and discharge, ordering supplies, and requesting lab tests. It provides the essential administrative framework that supports clinical care.
Integrated modules within EHRs that provide clinicians with evidence-based knowledge and patient-specific information to enhance decision-making.
Nursing Informatics Role: Nurses benefit from alerts for drug interactions, reminders for preventative screenings, and guidance from clinical protocols (e.g., sepsis protocols). CDSS helps reduce medical errors and improve patient safety.
mHealth refers to the use of mobile devices for healthcare services and information. In Uganda, with its widespread mobile phone penetration, mHealth is a transformative force, enabling nurses to extend their reach and enhance patient engagement.
A flexible mobile data collection platform that allows users to build custom apps. It can guide users through structured workflows and works offline.
Impact on Nursing: Nurses train and supervise VHTs to use CommCare apps to register households, track immunizations, screen for malnutrition, and deliver consistent health education messages.
A mobile health wallet that enables users to save, send, and receive funds specifically for healthcare expenses, connecting users, providers, and insurers.
Potential Impact for Uganda: Can reduce financial barriers to care, streamline payments for facilities, and enhance transparency. Nurses could interact with it for patient registration and verifying payment status.
Nursing informatics provides indispensable tools that are fundamentally transforming health research by streamlining data processes, enhancing data quality, and facilitating large-scale analysis.
Powerful platforms for electronic data capture. They allow researchers to design surveys digitally, deploy them on mobile devices for offline data collection, and then upload to a secure server.
Nursing Research Example: A nurse researcher studying maternal health in Mukono can use KoboToolbox on tablets to directly collect data from mothers, reducing errors and speeding up analysis to identify gaps in service delivery.
While primarily an aggregate reporting system, DHIS2 is a rich source of secondary data for health research.
Nursing Research Example: A researcher can analyze anonymized, aggregated DHIS2 data to investigate trends in childhood immunization coverage across Uganda, helping to identify areas with low coverage and inform public health nursing strategies.
Once data is collected electronically, it can be exported into specialized software for in-depth quantitative analysis.
Nursing Research Example: After collecting data via KoboToolbox, a nurse researcher can use STATA or R to perform rigorous statistical analysis, providing the empirical evidence needed to publish findings and influence policy.
Sister Callista Roy's Adaptation Model (RAM) is a prominent nursing theory that offers a powerful lens through which to understand how individuals and groups respond to environmental changes. It views the person as an adaptive system constantly interacting with a changing environment, striving to maintain physiological, psychological, and social integrity.
In nursing informatics, the introduction of new technology is a significant environmental "stimulus" that demands adaptation from nurses and students. Understanding these adaptive responses is crucial for successful technology implementation and for minimizing maladaptive outcomes like resistance or burnout.
The body's physical responses. Technology can trigger stressors like eye strain from prolonged screen time, headaches from cognitive load, and musculoskeletal issues from poor ergonomics.
One's sense of identity and self-esteem. A nurse might initially feel anxious or incompetent when confronted with a complex new EHR, impacting job satisfaction. Mastering the technology can significantly boost self-esteem.
The roles an individual occupies. Technology often redefines a nurse's professional role to include more data analysis, telehealth coaching, or remote monitoring, which can be empowering for some but threatening for others.
Relationships and social support systems. Technology can enhance collaboration through shared EHRs or create barriers if it leads to less face-to-face interaction or if systems are not interoperable.
Roy's model provides a systematic framework for nurses and educators to proactively facilitate positive adaptation to technological changes.
Before implementing new technology, a thorough assessment of psychological and social readiness is essential. Ask questions about perceptions, current competencies, and contextual factors like organizational culture and infrastructure.
Actionable Strategies:
Once needs are assessed, provide targeted interventions to facilitate positive adaptation by creating a supportive environment for learning and problem-solving.
Actionable Strategies:
Self-efficacy—the belief in one's capability to succeed—is critical for successful adaptation. This can be built through several methods.
Actionable Strategies:
By systematically applying Roy's Adaptation Model, nursing informatics professionals and educators can create more humane and effective strategies for integrating technology into nursing in Uganda, leading to improved patient outcomes and a more empowered nursing workforce.
A quiz on ICT in Health & Nursing Care.
1. Which of the following is NOT listed as an ICT tool used to enhance client education?
Correct (b): The definition of nursing informatics in client education explicitly lists mobile apps, SMS, videos, and patient portals. Fax machines are an older technology and are not mentioned in this context.
2. What ICT methodology is used at Mulago Hospital to teach mothers about kangaroo mother care?
Correct (c): The example for Mulago National Referral Hospital specifically mentions that nurses use "tablets with animations to teach mothers," which falls under multimedia education.
3. The use of SMS reminders for ART adherence at Reach Out Mbuya is an example of which methodology?
Correct (b): Sending SMS reminders for medication adherence is a classic example of a Mobile Health (mHealth) application.
4. How do nurses at the Uganda Heart Institute use videos to educate patients?
Correct (c): The text provides a specific example of multimedia education where "patients watch videos about lifestyle modification in waiting areas" at the Uganda Heart Institute.
5. Which of the following is a primary role of Nursing Informatics in discharge planning?
Correct (b): The core role in discharge planning is ensuring a safe transition by making sure patients understand their medications, follow-up, diet, and danger signs.
Incorrect: The other options relate to administration and research, not the direct patient transition process of discharge.
6. At Mbarara Hospital, what do nurses use to link printed discharge booklets to Ministry of Health guidelines?
Correct (b): The example for Mbarara Regional Referral Hospital explicitly states the use of "printed discharge booklets with QR codes linking to Ministry of Health guidelines."
7. What is a listed benefit of using nursing informatics in client education and discharge planning?
Correct (c): A key benefit is promoting continuity of care through tools like SMS reminders, telehealth follow-ups, and accessible patient portals.
Incorrect: Informatics aims to achieve the opposite of the other options: it reduces readmissions, strengthens communication, and improves patient self-care.
8. Which is a challenge for ICT in health & nursing care in rural health facilities?
Correct (c): A major challenge, especially in rural areas, is the lack of reliable internet, power, and necessary hardware, which is defined as limited ICT infrastructure.
Incorrect: The other options are the opposite of the listed challenges.
9. In the case study, what combination of actions by the nurse led to reduced readmissions and improved satisfaction?
Correct (b): The case study demonstrates a multi-faceted approach, combining multimedia education (video), clear documentation (summary), and mHealth follow-up (SMS) to achieve positive outcomes.
10. Which component of Information Systems (IS) is defined as "Designed to support nursing functions" by managing health data?
Correct (b): The description of collecting, storing, analyzing, and disseminating health data to support nursing functions refers to the core processes that these systems are designed to perform.
11. DHIS2, NextGen, and KoboToolbox are listed as examples of what in Uganda?
Correct (b): These are all explicitly listed under the heading "Information systems in nursing: In Uganda, examples include..."
12. What is mHealth primarily defined as in the provided text?
Correct (b): The definition provided for mHealth is "The use of mobile devices, SMS, mobile applications, and wireless technologies in healthcare."
13. Which ICT tool is mentioned for aggregating district health data for planning and monitoring?
Correct (c): Under "ICT Tools for Research," DHIS2 is specifically described as the tool that "Aggregates district health data for planning and monitoring."
Incorrect: REDCap is for field surveys, SPSS for analysis, and M-TIBA for healthcare financing.
14. What is a challenge identified for nursing informatics in health research?
Correct (d): The challenges section for health research explicitly lists "Data security and ethical concerns" as a key issue.
Incorrect: The other options are the opposite of the listed challenges.
15. Roy's Adaptation Theory applied to nursing informatics focuses on how to adapt to what?
Correct (b): The theory is applied to how nurses adapt to "technology stimuli" in their environment across all domains of practice.
16. The use of ICT to enhance the education of patients and caregivers is Nursing Informatics in _________ education.
17. Nurses at St. Francis Hospital Nsambya send follow-up _________ reminders for discharge medications.
18. One benefit of nursing informatics is that it promotes _________ of care through ICT follow-up.
19. A hospital's patient demographics, admissions, and billing are managed by a _________ Information System (HIS).
20. Roy's Adaptation Theory suggests fostering adaptive responses to technology through hands-on learning, support, and _________.
Your Score:
0%
0 / 0 correct
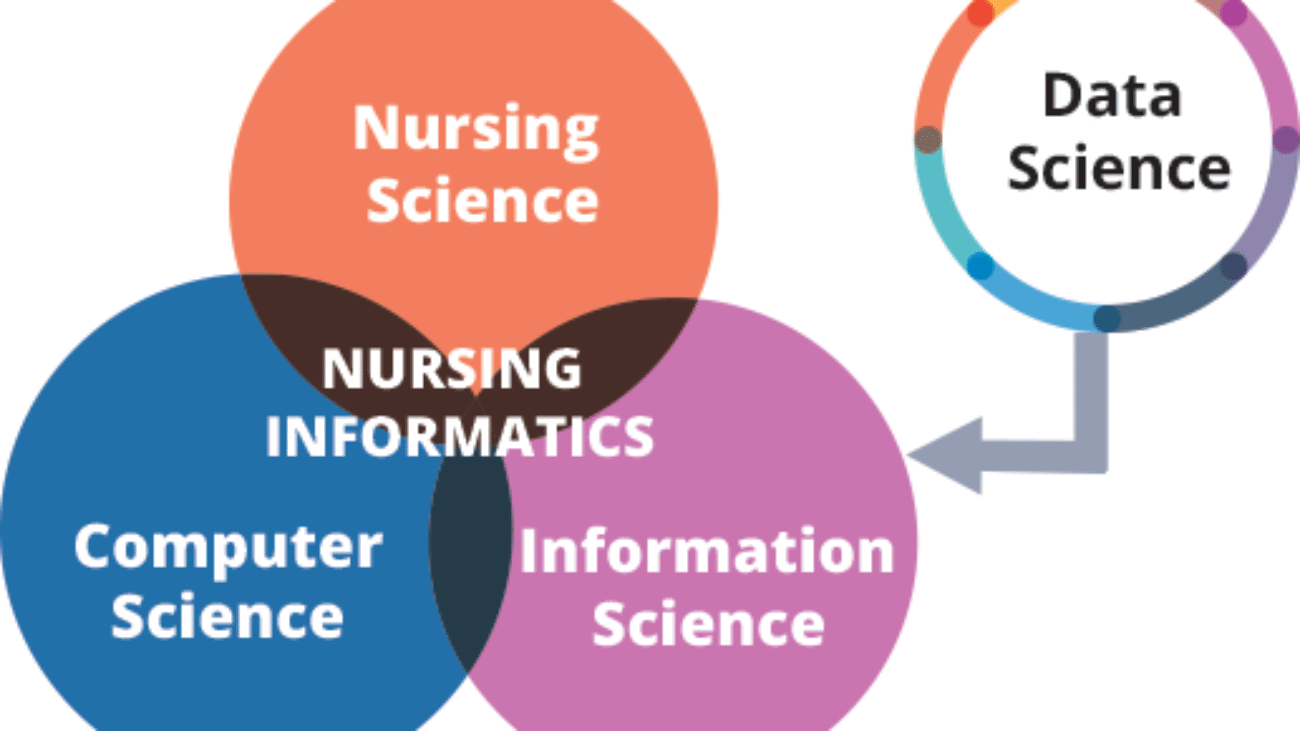
Theoretical models are like maps or blueprints that help us understand concepts. In nursing informatics, these models provide a framework for understanding and applying informatics principles, guiding how we think about data, manage change, and implement technology effectively in healthcare.
This is a foundational model, often depicted as a pyramid, illustrating how raw, unprocessed facts evolve into profound understanding and expert judgment. It's crucial for understanding the value proposition of nursing informatics – transforming simple observations into actionable wisdom for patient care.
Raw, isolated, and unprocessed facts without context or meaning. By itself, it doesn't tell a story or answer a question. Simplified: Just numbers, words, or observations.
Data that has been organized, structured, processed, or interpreted within a specific context. It answers "who," "what," "where," and "when." Data with meaning.
The synthesis of information, often through experience, education, and research, to identify relationships, patterns, and principles. It answers "how" to apply information and understand its implications. Understanding why something is happening and what it means.
The ability to apply knowledge, experience, and intuition with judgment to manage and solve problems effectively and ethically, especially in complex or novel situations. It involves understanding "why" to do something and "when" to do it, considering values and societal implications. Expert judgment and decision-making that leads to the best outcome.
This early and influential model provided a crucial conceptual framework for nursing informatics. It's often visualized as three overlapping circles (nursing science, computer science, information science) with data, information, and knowledge flowing through them, all directed towards supporting nursing practice. It was groundbreaking because it shifted the focus from merely using technology to understanding the purpose of information processing in nursing care.
Core Idea: Nursing informatics integrates the three core sciences to manage and process data, information, and knowledge effectively for the benefit of nursing practice.
The model was designed to provide a clear roadmap for nursing informatics with three primary goals:
The model works by systematically connecting the components. The following table shows a practical example of how to apply the model step-by-step:
| Steps | Examples in an Educational Context |
|---|---|
| Step 1: Identify the user and role. | User: Nurse Educator Role: Teaching |
| Step 2: Define the setting. | Setting: Nursing school or a university's skills lab. |
| Step 3: Clarify the goal. | Goal: Improve students’ skills and confidence in performing complex patient assessments. |
| Step 4: Apply knowledge & select technology. | Knowledge Base: Educational theory (e.g., experiential learning), clinical assessment guidelines, and best practices in simulation. Information Technologies: Select virtual simulation labs and interactive online case study platforms. |
| Step 5: Achieve the nursing outcome. | Outcome: Students practice assessments in a safe, repeatable virtual environment, leading to increased competency and better preparedness for real clinical settings. |
Implementing new technology, like a new EHR system or a telehealth platform, is a significant undertaking that requires careful management of human behavior and organizational processes. Understanding change theories is essential for successful adoption and minimizing resistance.
Kurt Lewin's classic model provides a simple yet powerful three-step process for managing planned change within an organization.
Preparing the organization or individuals for change by creating awareness of why the old way of doing things is no longer sufficient and establishing a felt need for change. It involves breaking down old habits and assumptions. Convincing everyone that the old way isn't working and a new way is needed.
Expanded Example: A hospital management team presents compelling data on the high rates of medication errors, documentation inefficiencies, and patient complaints linked to the current paper-based charting system. They hold town hall meetings and workshops, actively involving nursing staff, to discuss the critical need for a new EHR system to improve patient safety, streamline workflows, and enhance overall quality of care. They highlight the financial and reputational costs of not changing.
The actual implementation phase where the change occurs. This stage involves significant training, communication, support, and adaptation as people learn new processes and tools. Rolling out the new system and teaching everyone how to use it.
Expanded Example: The new EHR system is rolled out systematically, perhaps unit by unit or department by department. Intensive, hands-on training sessions are conducted for all nursing staff. Specially trained "super-users" (nurses proficient in the new system) are deployed on the floors to provide immediate, peer-to-peer support. The IT department establishes a dedicated 24/7 help desk. Regular feedback sessions are held to identify and quickly address any technical glitches or workflow issues.
Stabilizing the change and making it the new standard practice. This involves integrating the new methods into the organizational culture, updating policies, and reinforcing the benefits of the change. Making the new way the permanent, normal way of doing things.
Expanded Example: New hospital policies and procedures are formally established that mandate the exclusive use of the EHR for all patient documentation and order entry. Leadership publicly celebrates early successes (e.g., reduction in medication errors, improved documentation compliance). Ongoing refresher training is provided for new hires and to address advanced features. Audits are performed to ensure compliance, and the use of the EHR becomes deeply embedded in the daily workflow, becoming the "new normal."
Everett Rogers' theory examines how new ideas, technologies, or practices spread through a social system over time. It's particularly useful for understanding how different groups of people adopt innovations at different rates, allowing for tailored communication and implementation strategies.
These are the first to adopt new ideas, often risk-takers and enthusiasts. They are eager to experiment.
Role: Often seek out new technology and are willing to try it even if it's not perfect.
Example: When a new telehealth platform is introduced in a Ugandan district, an innovator nurse might be the first to volunteer for the pilot program, eager to test its capabilities and provide early feedback, even if internet connectivity is sometimes challenging.
Respected opinion leaders within the community or profession. They adopt new ideas early but with more thought and evaluation than innovators. They are crucial for influencing the broader group.
Role: Act as role models and champions, legitimizing the innovation.
Example: Other experienced and well-respected nurses in the district watch the innovators. Seeing the benefits, an early adopter nurse begins using the telehealth platform and actively champions its use to their peers, sharing their positive experiences and insights during staff meetings.
Deliberate individuals who adopt new ideas just before the average person. They need to see evidence that the innovation works and is useful.
Role: They make the innovation mainstream.
Example: After seeing positive results and hearing positive feedback from the early adopters, the majority of nurses in the district begin to adopt the telehealth platform, recognizing its practical benefits for patient care and convenience.
Skeptical individuals who will only adopt an innovation after a majority of people have tried it and it has become widely accepted. They are often influenced by peer pressure or economic necessity.
Role: Their adoption signals widespread acceptance.
Example: Some nurses are hesitant and prefer traditional methods. They only begin to use the telehealth platform when it becomes an established and expected part of routine practice, perhaps after a mandate or when training and support are widely available.
Traditionalists who are the last to adopt an innovation. They are often resistant to change, prefer traditional methods, and have little to no opinion leadership.
Role: May only adopt when older options are no longer available.
Example: A few nurses may resist using the telehealth platform until there's virtually no other option for certain consultations or if their traditional methods become unsustainable. They might require significant individual support and encouragement.
Application: Understanding these categories helps implementers tailor their communication, training, and support strategies to each group to maximize adoption.
This theory views any organization, like a hospital, a clinic, or even a patient's body, as a complex system. It posits that a system is made up of many interconnected parts (subsystems) that work together to achieve a common goal. A key tenet is that a change in one part of the system will inevitably affect all other parts, highlighting the importance of a holistic perspective.
Core Idea: Everything is connected. When you change one thing in a system, it impacts everything else.
Resources, information, or energy entering the system from its environment.
Example: Patient demographic data, lab results, nurse staffing levels, available IT infrastructure (computers, internet connectivity), medical supplies.
The activities or work done within the system to transform the input.
Example: Nurses and doctors entering and processing patient data within the EHR, administering medications, performing patient assessments, collaborating with other departments, and making clinical decisions.
The products, services, or outcomes that result from the system's processes.
Example: A complete and accurate patient health record, clinical decision support alerts, patient discharge summaries, billing information, improved patient outcomes (e.g., reduced readmission rates).
Information about the system's output that is fed back into the system to make adjustments, correct errors, and improve future performance.
Example: Nurses report that a specific screen in the EHR is confusing or takes too long to complete, leading to a system modification by the IT team. Patient satisfaction surveys, infection rates, or medication error reports provide feedback on the quality of care delivered.
External factors, conditions, or influences that interact with and affect the system but are largely outside its direct control.
Example: Government regulations (e.g., data protection laws like Uganda's Data Protection and Privacy Act, or international standards like HIPAA), economic conditions, technological advancements, patient demographics, public health crises (like an epidemic), and relationships with technology vendors.
When implementing a new EHR in a large hospital through a systems lens:
| Concepts | Example: Implementation of an EHR |
|---|---|
| System | Hospital’s health information infrastructure. |
| Input | Patient data (demographics, vitals, lab results), staff expertise, IT resources. |
| Throughput (Process) | Data entry, storage, processing, and analysis within the EHR system. |
| Output | Patient charts, clinical decision support alerts, discharge summaries. |
| Feedback | User satisfaction surveys, system usage reports, error rates. |
| Environment | Government regulations, technology vendors, patient needs, and funding. |
| Open vs. Closed Systems |
Open Systems:
|
This module explores the tangible benefits that nursing informatics brings to healthcare and introduces the crucial role of the Nurse Informaticist, the specialist who drives many of these advancements.
Nursing informatics isn't just about using computers; it's about fundamentally transforming healthcare for the better. Here are some of its most significant impacts:
Historically, vast amounts of clinical data were locked away in paper charts, making it incredibly difficult to analyze or learn from. Informatics systems (like EHRs) digitize this data, allowing it to be easily searched, aggregated, and analyzed. Turns piles of paper notes into smart insights.
Expanded Example: Instead of manually sifting through hundreds of patient files to find out how many patients with malaria responded to a specific treatment, an informaticist can query the EHR. This data can then be used for quality improvement projects (e.g., "Are we giving the right malaria treatment?") or for research. In a broader sense, this data can inform public health strategies in Uganda by showing patterns of disease outbreaks or the effectiveness of vaccination campaigns across different districts.
Informatics systems are designed with patient safety at their core, significantly reducing the potential for human error. Built-in safeguards prevent mistakes.
Expanded Examples: Barcode Medication Administration (BCMA) provides a crucial safety net. Clinical Decision Support (CDS) Alerts can automatically flag a severe drug allergy or a dangerous drug-drug interaction. Eliminating illegible handwriting ensures all care providers are working with accurate information.
Informatics systems capture the data needed to demonstrate quality outcomes and cost-effectiveness to insurance companies, government agencies, and donors. Shows proof of good care and efficient spending.
Expanded Example: A hospital can easily generate reports showing its infection rates or patient readmission rates. In Uganda, this could mean demonstrating to the Ministry of Health that specific health interventions are effective and resources are being used wisely, leading to continued funding and support.
The digital nature of EHRs eliminates the physical space, security risks, and retrieval delays associated with paper charts. Information can be accessed instantly from multiple locations simultaneously. No more lost charts or endless searching; everything is a click away.
Expanded Example: Instead of searching through dusty paper archives, a nurse can access a patient's medical history instantly from a workstation or mobile device, even if the patient was last seen years ago. This is highly beneficial where maintaining a continuous paper record is challenging.
By streamlining workflows, reducing redundant tests, preventing errors, and improving efficiency, informatics contributes significantly to cost savings and better resource utilization. More efficient care, fewer wasted resources.
Expanded Example: Reduced time spent on documentation means nurses have more time for direct patient care. Preventing a medication error avoids the costs associated with extended hospital stays and additional treatments. Electronic ordering of tests and medications reduces errors and speeds up processes.
A Nurse Informaticist (NI) is a highly specialized registered nurse who possesses a deep understanding of both clinical nursing practice and information technology. They are critical to successful technology integration in healthcare, acting as the indispensable link between the worlds of nursing and IT.
Play a central role in bringing new clinical information systems into an organization, from evaluation and customization to rollout.
Example: When a hospital in Kampala upgrades its EHR, the NI leads requirements gathering from nurses, works with vendors to configure the system for local practices, designs workflows, and oversees testing and go-live.
Analyze existing clinical processes and identify areas where technology can make them more efficient, safer, and user-friendly.
Example: An NI might observe nurses spending too much time navigating the EHR to document vitals. They would then work with IT to streamline the process by creating a consolidated "daily care" screen, reducing charting burden.
Develop and deliver comprehensive training programs for all nursing staff on how to use technology effectively and serve as a primary resource for troubleshooting.
Example: After a new patient monitoring system is installed, the NI will design and lead hands-on training, create user guides, and be on-site during go-live to provide immediate support.
Extract, interpret, and present data from clinical systems to identify trends, monitor quality metrics, and support research.
Example: An NI might analyze EHR data to identify a correlation between a specific staffing model and patient fall rates, providing evidence for practice changes. In public health, they might analyze vaccination rates against disease incidence.
Develop and update organizational policies related to the secure and ethical use of clinical information systems, including data privacy and security.
Example: The NI will ensure the hospital's policies for accessing EHR data comply with national data privacy laws, developing clear guidelines on what information nurses can share and how to handle sensitive data.
As technology becomes more ingrained in nursing, every nurse needs a foundational understanding of informatics. This module highlights the essential competencies and the critical ethical responsibilities that come with managing patient data.
It's not just Nurse Informaticists who need informatics skills; all nurses require a baseline level of competency. The TIGER (Technology Informatics Guiding Education Reform) Initiative provides a widely recognized framework:
The fundamental ability to use computers and software. Knowing how to use a computer. This includes using a keyboard, navigating operating systems, sending emails, and basic file management.
The ability to find, evaluate, and use relevant information. Knowing how to find good information and tell if it's trustworthy. This includes searching databases like PubMed and critically evaluating online sources.
The ability to use clinical information systems like the EHR. Knowing how to use patient record systems effectively. This includes documenting care, retrieving data, and using decision support tools.
The power of digital health information comes with significant ethical responsibilities. Nurses are trusted custodians of patient data.
Protecting sensitive patient information from unauthorized access or misuse. Keeping patient information secret. This means never sharing data without consent and being mindful of who can see or hear information.
Implementing safeguards to protect electronic health information from being lost, stolen, or corrupted. Protecting patient data from hackers and mistakes. This includes using strong passwords and logging out of systems.
Ensuring that the data being entered, stored, and retrieved is accurate, complete, and reliable. Making sure patient records are always correct. Inaccurate data can lead to serious patient harm.
This module provides an opportunity for personal reflection on the material covered and looks ahead to the exciting and rapidly evolving future of nursing informatics.
Take a moment to pause and consider how the concepts we've discussed apply to your own experiences and aspirations in nursing.
The field of nursing informatics is dynamic and constantly evolving. Here are some key trends that will shape its future:
The use of technology to deliver healthcare remotely. Expect a continued surge in virtual appointments and remote patient monitoring, which is transformative for extending healthcare access to underserved rural populations, a significant benefit in Uganda.
Analyzing enormous volumes of healthcare data to identify patterns, predict outcomes, and guide interventions. Nurses will use this to identify high-risk patients for events like sepsis or falls before they occur, allowing for proactive, personalized care.
AI will integrate into clinical decision support, offering sophisticated guidance on diagnoses and treatment plans. It may also automate routine documentation, freeing up nurses for more direct patient interaction.
Empowering patients to take a more active role in their health through advanced patient portals, mobile health apps (mHealth), and wearable devices. Nurses will be key in educating patients on how to use these tools effectively.
The ability of different healthcare systems to communicate and exchange data seamlessly. The goal is for a patient's health information to follow them effortlessly across all providers, reducing redundant tests and improving care coordination.
A quiz on Theoretical Models in Nursing Informatics.
1. In the DIKW Pyramid, what is defined as "raw facts without context"?
Correct (c): "Data" is explicitly defined as "Raw facts without context."
Incorrect (a): Information is organized data with meaning.
Incorrect (b): Knowledge is synthesized information for decision-making.
Incorrect (d): Wisdom is applying knowledge effectively.
2. According to the DIKW Model, when is information combined with nursing experience and evidence?
Correct (c): Knowledge is formed when information is combined with nursing experience and evidence (e.g., knowing high BP increases cardiovascular risk).
Incorrect (b): Wisdom is the application of knowledge.
3. Which of the following would be an example of 'Wisdom' in the DIKW Pyramid?
Correct (d): Wisdom is applying knowledge to make a sound decision, such as creating a personalized care plan based on identified risks.
Incorrect (a): This is Data.
Incorrect (b): This is Information.
Incorrect (c): This is Knowledge.
4. The Graves & Corcoran Model (1989) describes the key components for nurses to effectively use what?
Correct (c): The model explicitly "describes the key components and relationships needed for nurses to effectively use information systems in healthcare."
5. Which of the following is NOT listed as a main component of the Graves & Corcoran Model?
Correct (c): The main components listed are Users, Roles, Settings, Goals, Knowledge Base, and Information Technologies. Funding is not a core component of the model itself.
6. In the Graves & Corcoran Model, which step involves applying the knowledge base and selecting technologies?
Correct (d): The model's flow clearly outlines Step 4 as "Apply the knowledge base and select the right information technologies."
7. Roger's Diffusion of Innovation Theory is categorized as which type of change?
Correct (b): Roger's theory describes how innovations spread naturally through a social system, which is considered an "unplanned" pattern of change.
Incorrect (a): Lewin's Change Theory is an example of a "planned" change model.
8. According to Roger's theory, which category of adopters are opinion leaders and promoters?
Correct (b): Early adopters are described as "opinion leaders who function as promoters of innovation."
Incorrect (a): Innovators are the very first to adopt but are a smaller group.
Incorrect (c): The early majority are averse to risks.
Incorrect (d): Laggards are suspicious and resistant to change.
9. The "Late majority" in Roger's theory typically needs what before adopting an innovation?
Correct (b): The late majority are skeptical and require proof that the innovation is beneficial and has been adopted by many others before they will consider it.
10. Which step in Lewin's Change Theory involves preparing people and explaining why change is needed?
Correct (a): "Unfreezing" is the initial step where awareness is created, and people are prepared to move away from the current state.
Incorrect (b): Moving is the implementation phase.
Incorrect (c): Refreezing is about sustaining the change.
11. Providing hands-on training and user support during a new system implementation falls under which step of Lewin's theory?
Correct (b): The "Changing (Moving)" step is the transition phase where the new system is rolled out, and users are provided with training and support.
12. What is the goal of the 'Refreezing' step in Lewin's Change Theory?
Correct (c): The goal of "Refreezing" is to stabilize the change and integrate it into the normal workflow to ensure it becomes permanent.
Incorrect (a): This is the goal of Unfreezing.
Incorrect (b): This is the goal of Moving.
13. In General Systems Theory, what is "Resources, information, or energy entering the system"?
Correct (d): "Input" is defined as "Resources, information, or energy entering the system."
Incorrect (a): Output is what is generated by the system.
Incorrect (b): Throughput is how inputs are transformed.
Incorrect (c): Feedback is information about performance.
14. User satisfaction surveys and system usage reports are examples of what concept in General Systems Theory?
Correct (c): "Feedback" is "Information about the system’s performance used to make adjustments," which perfectly describes surveys and reports.
15. An EHR connecting with labs, pharmacies, and insurance is an example of what type of system?
Correct (c): An open system interacts with its environment. The EHR interacting with external entities like labs and pharmacies is a prime example.
Incorrect (a): Closed systems are self-contained and do not interact with their environment.
16. In the DIKW Pyramid, _______ is defined as synthesized information for decision-making.
17. The Graves & Corcoran Model shows how informatics helps nurses achieve goals in patient care, education, research, and _________.
18. Adopters in Roger's theory who are suspicious of innovation and very intractable are known as _________.
19. Lewin's Change Theory involves a three-step process: Unfreezing, Moving (changing), and _________.
20. In General Systems Theory, external factors like government regulations are referred to as the _________.
Your Score:
0%
0 / 0 correct
Upon completing this module, you will be able to:
Imagine a nurse taking care of a patient. Traditionally, this involved paper charts, handwritten notes, and verbal updates. Now, picture that same nurse using a tablet to access a patient's full medical history instantly, scanning a barcode on medication before administering it, or even using a telehealth app to check in with a patient remotely. This powerful blend of nursing care with technology is what we call Nursing Informatics.
At its heart, nursing informatics is the specialty that combines the art of nursing (your skills, knowledge, and compassion) with the power of computer and information sciences (technology and how we organize information).
The American Nurses Association (ANA) offers a formal definition that helps us understand it better: it's "the integration of nursing science, computer science, and information science to manage and communicate data, information, knowledge, and wisdom in nursing practice."
In simpler terms: Think of nursing informatics as the bridge between the clinical side of nursing and the technological tools used to deliver and document care. This field ensures that technology truly serves the needs of nurses and patients, making healthcare safer, more efficient, and ultimately, more effective.
Example: Consider a remote health clinic in Uganda. Nursing informatics isn't just about having a computer; it's about how that computer helps a nurse track patient vaccinations, manage drug inventory digitally, or even connect via video call with a specialist in Kampala for advice on a complex case.
Nursing informatics stands on three essential scientific pillars:
This is the foundation – the clinical knowledge, critical thinking, judgment, and patient care skills that every nurse possesses. It's what nurses do and why they do it. It encompasses understanding diseases, patient responses, care planning, and therapeutic interventions.
Example: A nurse recognizing the signs of malaria, knowing the appropriate nursing interventions, and understanding patient education needs. This clinical expertise guides how technology should be designed and used.
This involves the tools themselves – the hardware (physical computers, tablets, servers), software (applications, operating systems), and the underlying systems (networks, databases) that manage and process data. It's how the technology works.
Example: The Electronic Health Record (EHR) system that stores all patient data, the internet connection enabling telehealth, or the barcode scanner used for medication administration.
This focuses on how data is collected, organized, stored, retrieved, interpreted, and used to create meaningful information that supports decision-making. It's about making sense of the data. It's about turning raw facts into useful insights.
Example: Instead of just having a list of patient temperatures (data), information science helps organize these temperatures over time into a graph (information) that clearly shows a fever trend, allowing the nurse to understand the patient's condition better and make decisions.
Nursing informatics is not confined to the hospital ward or patient's bedside. Its principles and applications extend across all domains of the nursing profession, influencing every aspect of healthcare.
This is the most visible area, where informatics directly supports nurses in providing patient care.
Examples:
Informatics plays a crucial role in training the next generation of nurses and continuously educating current practitioners. How technology helps nurses learn and stay updated.
Examples:
Nurse leaders and managers use informatics tools to manage resources, monitor quality, and make strategic decisions for healthcare organizations. How technology helps manage hospitals, clinics, and nursing staff.
Examples:
Informatics provides powerful tools for nursing researchers to collect, analyze, and interpret large datasets, advancing nursing science and evidence-based practice. How technology helps nurses discover new knowledge and improve care through studies.
Examples:
The integration of informatics into nursing is not just a trend; it's essential for modern healthcare.
By providing nurses and other clinicians with quick, accurate, and comprehensive access to a patient's complete medical history, including allergies, current medications, past diagnoses, and lab results, informatics significantly reduces the risk of medical errors. Keeps patients safer by preventing mistakes.
Informatics systems can embed the latest clinical guidelines, best practices, and research findings directly into the clinical workflow. This helps nurses make decisions based on the most current and credible evidence available, rather than tradition or anecdote. Ensures nurses use the best, most proven methods of care.
Well-designed informatics systems streamline documentation, reduce redundant data entry, and automate many administrative tasks. This frees up nurses' valuable time, allowing them to focus more on direct patient care and less on paperwork. Saves nurses time and makes their work smoother.
Integrated EHRs and communication platforms allow for seamless and timely communication among the entire healthcare team—nurses, doctors, pharmacists, therapists, and even the patient. Everyone has access to the most current patient information, reducing misunderstandings and improving coordinated care. Helps everyone involved in patient care talk to each other and share information easily.
Informatics aggregates vast amounts of clinical data from many patients. When this data is anonymized, it can be analyzed to spot trends, measure the effectiveness of treatments, and improve care processes across the entire organization or community. Helps hospitals learn from data and protect community health.
Modern informatics tools often include patient-facing components, like online portals. These tools give patients direct access to their own health information, turning them from passive recipients of care into active partners in managing their health. Gives patients tools to be more involved in their own healthcare.
An Introduction to Nursing Informatics.
1. Which of the following best describes the core concept of Nursing Informatics?
Correct (b): Nursing informatics is the specialty that combines the art of nursing (skills, knowledge) with the power of computer and information sciences.
Incorrect (a, c, d): These options are too narrow. While informatics involves troubleshooting, software, and communication, its core is the integration of these three specific sciences.
2. According to the ANA, Nursing Informatics involves the integration of which three sciences?
Correct (b): The ANA definition explicitly states the integration of "nursing science, computer science, and information science."
Incorrect (a, c, d): These options do not match the specific terms used in the official ANA definition.
3. Which is an example of 'Nursing Science' within the context of Nursing Informatics?
Correct (b): Nursing Science encompasses the clinical knowledge, critical thinking, judgment, and patient care skills that every nurse possesses.
Incorrect (a): This is Computer Science.
Incorrect (c): This is a mix of Computer and Information Science.
Incorrect (d): This is Information Science.
4. Which pillar is concerned with hardware, software, networks, and databases?
Correct (c): Computer Science involves the tools themselves – the hardware, software, and underlying systems that manage and process data.
5. Converting a list of patient temperatures into a fever trend graph is an example of what science?
Correct (c): Information Science is about organizing raw data (temperatures) into meaningful information (a trend graph) to support decision-making.
6. Barcode Medication Administration (BCMA) systems most directly support which domain of Nursing Informatics?
Correct (c): BCMA systems directly support nurses in providing safe patient care at the bedside, which is the core of the "Practice" domain.
7. A nurse using telehealth for a virtual consultation exemplifies informatics in which domain?
Correct (d): Telehealth platforms are a key tool for direct patient care, allowing nurses to conduct virtual consultations and monitor patients remotely, placing it firmly in the "Practice" domain.
8. Training students in a virtual simulation lab falls under which scope of Nursing Informatics?
Correct (b): Virtual simulation labs are educational tools that allow students to practice clinical scenarios in a safe, controlled digital environment.
9. Using a quality improvement dashboard to visualize metrics like infection rates is an example of informatics in which domain?
Correct (c): Dashboards that visualize key performance indicators help managers and administrators make strategic decisions to improve quality and safety, which is a core function of the "Administration" domain.
10. Extracting anonymized patient data from EHRs to identify disease trends is an application of informatics in which domain?
Correct (d): Using large sets of anonymized data from EHRs to analyze trends, evaluate treatments, and study disease patterns is a primary function of the "Research" domain in nursing informatics.
11. Which is a highlighted benefit of informatics in improving patient safety?
Correct (b): Quick, comprehensive access to a patient's history, allergies, and medications, along with real-time alerts, significantly reduces the risk of medical errors.
Incorrect: Informatics supports, not replaces, clinical judgment and communication. It assists, not automates, decisions.
12. The "five rights" of medication administration are significantly enhanced by which system?
Correct (c): BCMA systems, by requiring scans of the patient's wristband and the medication barcode, directly verify the "five rights" at the point of care, dramatically reducing errors.
13. How does informatics contribute to evidence-based practice (EBP)?
Correct (b): Informatics systems can embed the latest clinical guidelines and best practices directly into the clinical workflow, helping nurses make decisions based on the most current evidence.
Incorrect: Informatics supports, not replaces, clinical judgment. It makes research more accessible, not obsolete.
14. Which example best illustrates how informatics enhances workflow efficiency?
Correct (b): Automating tasks like charting vital signs eliminates manual entry, saves time, reduces errors, and improves overall workflow efficiency.
Incorrect: The other options describe inefficient, error-prone, or outdated workflows that informatics aims to improve.
15. One key way informatics facilitates better communication and collaboration is through:
Correct (c): A shared, up-to-date patient record allows all members of the care team to see the same information, which is fundamental to effective collaboration.
Incorrect: The other options describe information silos or practices that hinder communication and collaboration.
16. Nursing informatics combines nursing science with _________ and information sciences.
17. An EHR system and barcode scanner are tools of the _________ science pillar.
18. Organizing raw temperatures into a fever trend graph is an application of _________ science.
19. The domain of nursing informatics involving staff scheduling and budget management is _________.
20. Clinical Decision Support (CDS) tools help nurses make _________ decisions by providing real-time alerts and guidance.
Your Score:
0%
0 / 0 correct
Nerve and muscle physiology is a branch of physiology that specifically studies the function and mechanisms of nervous tissue (nerves) and muscle tissue (muscles).
It explores how these "excitable tissues" generate and transmit electrical signals (like action potentials) and how these electrical signals are converted into specific cellular functions.
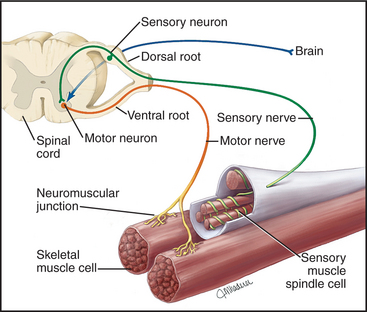
It covers how neurons (nerve cells) generate electrical impulses, communicate with each other (synaptic transmission), process information, and transmit signals throughout the body to control various functions, from thought and sensation to movement and organ regulation.
It focuses on how muscle cells (fibers) respond to electrical signals from nerves, leading to contraction (shortening) and the generation of force. This includes the molecular mechanisms of contraction, the regulation of muscle force, and the different types of muscle tissue and their distinct functional characteristics.
Nervous system excitability is the ability of nerve cells (neurons) to respond to a stimulus by generating and propagating an action potential, a self-propagating electrical impulse.
This property is fundamental to the nervous system's function and depends on the neuron's membrane's selective permeability, ion channels, and pumps. A change in membrane potential can lead to this event, which is essential for transmitting information throughout the body. The physiology of the nervous system involves its main divisions (the Central Nervous System (CNS) and Peripheral Nervous System (PNS)), which use neurons and electrochemical signals to sense stimuli, integrate information, and produce coordinated responses.
A motor neuron is a specialized nerve cell that transmits electrical signals from the central nervous system (brain and spinal cord) to muscles or glands, thereby initiating movement or secretion. It acts as the "final common pathway" by which the nervous system controls effector organs.
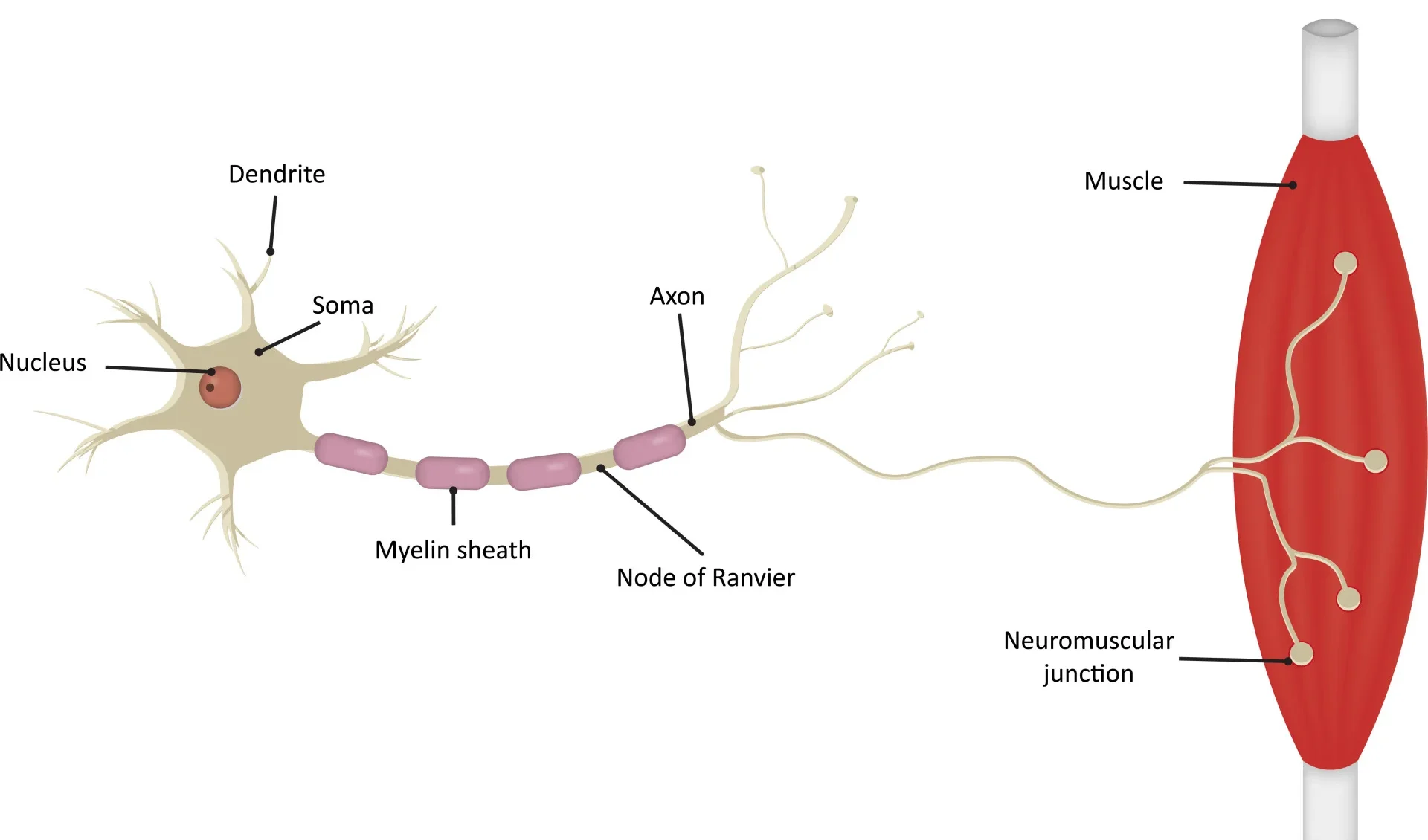
The metabolic center of the neuron, containing the nucleus and other organelles. It synthesizes neurotransmitters and proteins and receives synaptic inputs from other neurons.
Branching, tree-like extensions that are the primary receptive (input) regions. They contain ligand-gated ion channels that receive chemical signals and generate graded potentials (EPSPs and IPSPs).
A cone-shaped region where the axon originates. This is the critical "trigger zone" with the highest density of voltage-gated Na⁺ channels. It integrates all incoming potentials, and if the sum reaches threshold, an action potential is generated.
A single, long projection that transmits the action potential (the output signal) away from the cell body. Its length can exceed a meter.
A fatty, insulating layer that surrounds many axons, formed by Schwann cells in the PNS and oligodendrocytes in the CNS. It is crucial for increasing the speed of action potential conduction.
Gaps in the myelin sheath that contain a high concentration of voltage-gated Na⁺ and K⁺ channels. The action potential is regenerated at these nodes, "jumping" from one to the next in a process called saltatory conduction.
The branched ends of the axon that form synapses with other cells. They contain synaptic vesicles filled with neurotransmitters and are specialized for converting the electrical signal (action potential) into a chemical signal (neurotransmitter release).
We can map these anatomical components to four distinct functional zones, illustrating the flow of information:
Motor neurons are often referred to as the "final common pathway" in motor control. This term emphasizes a fundamental principle: all the complex neural computations happening in higher brain centers (e.g., planning and coordination in the cerebral cortex, basal ganglia, and cerebellum) ultimately converge onto these lower motor neurons.
It is only through the firing of a lower motor neuron that a skeletal muscle can be activated and a movement can occur. Regardless of whether a movement is voluntary or reflexive, the command signal ultimately travels down a lower motor neuron to its target muscle fibers. This makes the motor neuron a critical bottleneck and the ultimate determinant of muscle activity and all bodily movements.
Synaptic transmission is the fundamental process by which one neuron (the presynaptic neuron) communicates with another neuron (the postsynaptic neuron) or an effector cell. Most synapses in the nervous system are chemical synapses, meaning they utilize chemical messengers called neurotransmitters to bridge the microscopic gap between cells.
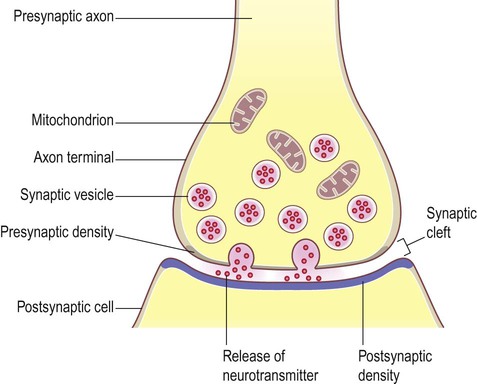
A chemical synapse consists of three main components:
Neurotransmitters are synthesized via distinct pathways and then packaged into synaptic vesicles. This packaging protects them from degradation, concentrates them for efficient release, and ensures their availability.
This phase converts the electrical signal into a chemical signal:
Once in the cleft, neurotransmitters diffuse across and bind reversibly to their specific receptors on the postsynaptic membrane, causing a response.
The receptor itself is an ion channel. Binding of the neurotransmitter causes an immediate opening, allowing ion flow and a rapid change in the postsynaptic membrane potential. This can generate:
The receptor activates an intracellular G-protein, which then initiates a slower but more widespread and long-lasting signaling cascade. This can lead to:
These events generate graded potentials (EPSPs or IPSPs). If the combined effect of these graded potentials at the axon hillock reaches threshold, a new action potential is triggered in the postsynaptic neuron.
To ensure precise and discrete signaling, the action of neurotransmitters must be swiftly terminated. This happens through several mechanisms:
The motor neuron is constantly bombarded with chemical signals from thousands of other neurons. These signals cause small, localized changes in the membrane potential, which the neuron must integrate to decide whether to fire an "all-or-nothing" action potential.
When a presynaptic neuron releases neurotransmitters, they bind to ligand-gated ion channels on the motor neuron, leading to a change in its membrane potential.
A depolarization of the postsynaptic membrane, making it less negative and more likely to fire. Typically caused by the influx of positive ions, most commonly Na⁺, when an excitatory neurotransmitter (e.g., glutamate) binds.
A hyperpolarization or stabilization of the membrane potential, making it more negative and less likely to fire. Typically caused by the influx of negative ions (Cl⁻) or the efflux of positive ions (K⁺) when an inhibitory neurotransmitter (e.g., GABA, glycine) binds.
A single EPSP is usually too weak to trigger an action potential. Motor neurons integrate thousands of inputs:
The axon hillock acts as the integrator. If the algebraic sum of all incoming EPSPs and IPSPs reaches the threshold potential (typically around -55 mV), an action potential is generated.
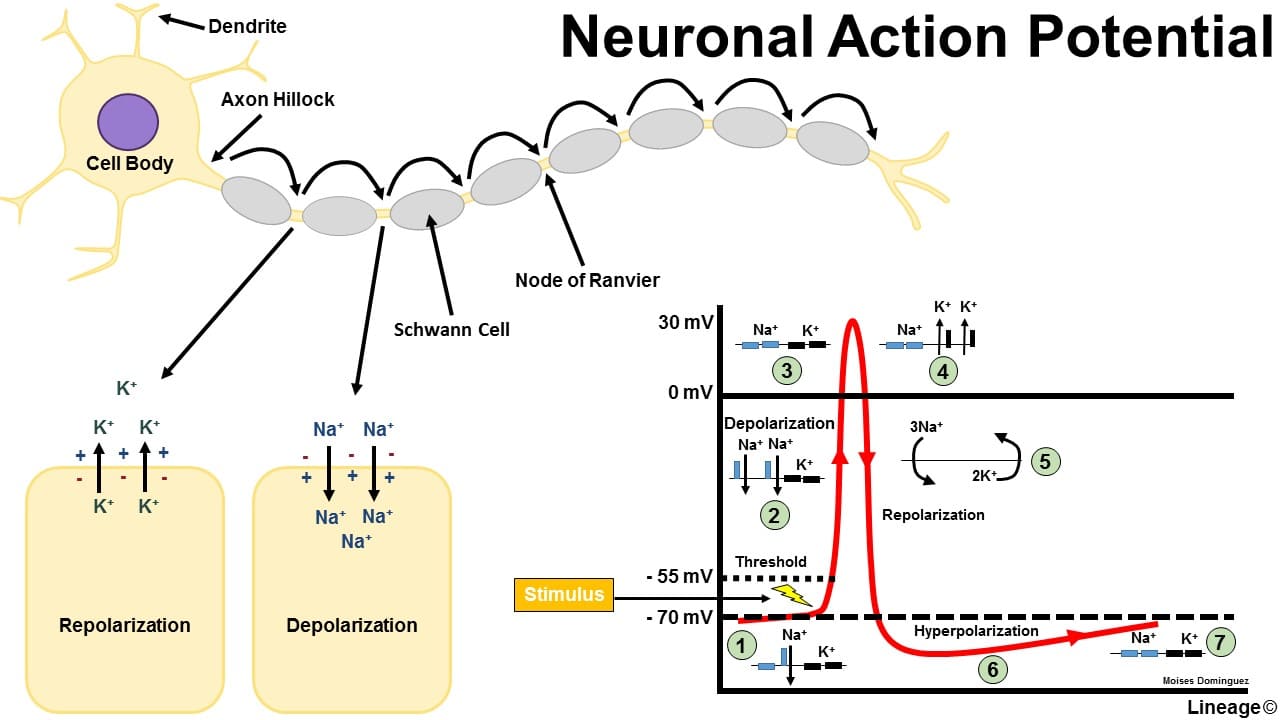
Once generated at the axon hillock, the action potential propagates along the axon without losing strength.
Muscle tissue is specialized for contraction, generating force and movement. Here, we'll focus on skeletal muscle.
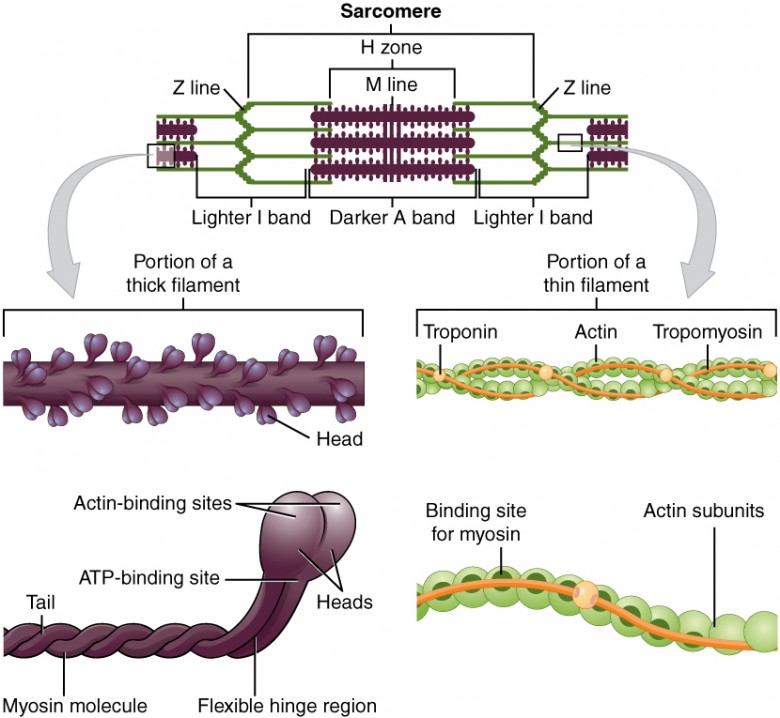
The sarcomere is the fundamental, repeating contractile unit of a myofibril, extending from one Z-disc to the next.

The neuromuscular junction (NMJ) is the specialized chemical synapse where a motor neuron's axon terminal meets a skeletal muscle fiber.
This is the muscle's initial, graded electrical response at the motor end plate:
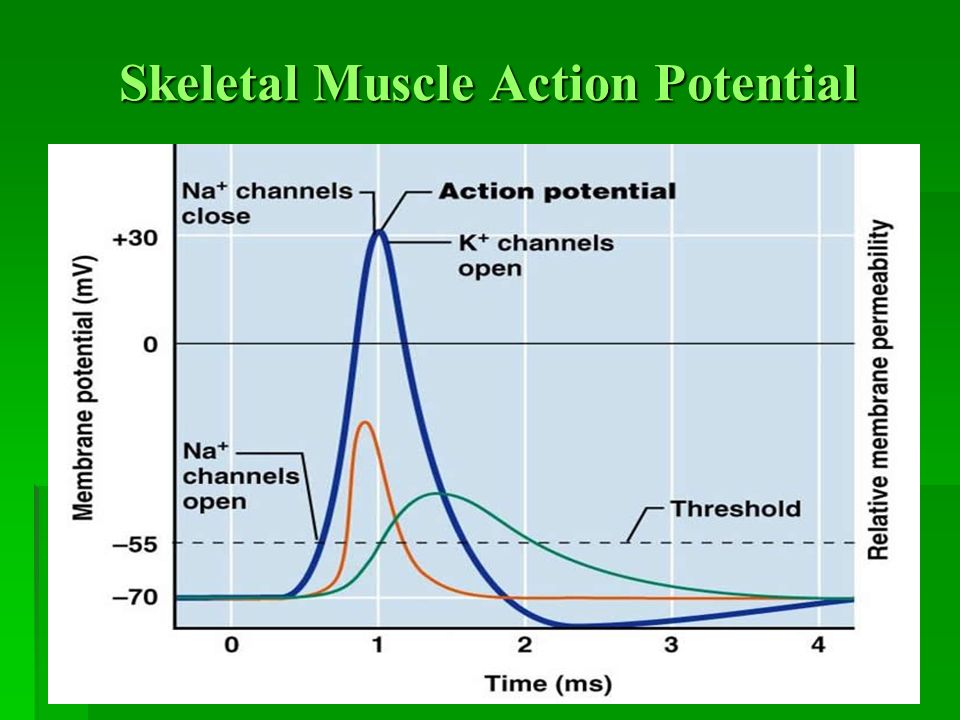
The muscle action potential is an "all-or-nothing" electrical signal that rapidly spreads across the entire muscle fiber membrane. Its characteristics are very similar to the neuronal action potential, but its purpose is specifically to initiate muscle contraction.
The muscle action potential propagates in two critical ways:
This is the physiological process by which an electrical signal (the muscle action potential) is converted into a mechanical event (muscle contraction).
The Sliding Filament Theory proposes that muscle shortening occurs by the thick and thin filaments sliding past one another, thereby increasing their overlap.
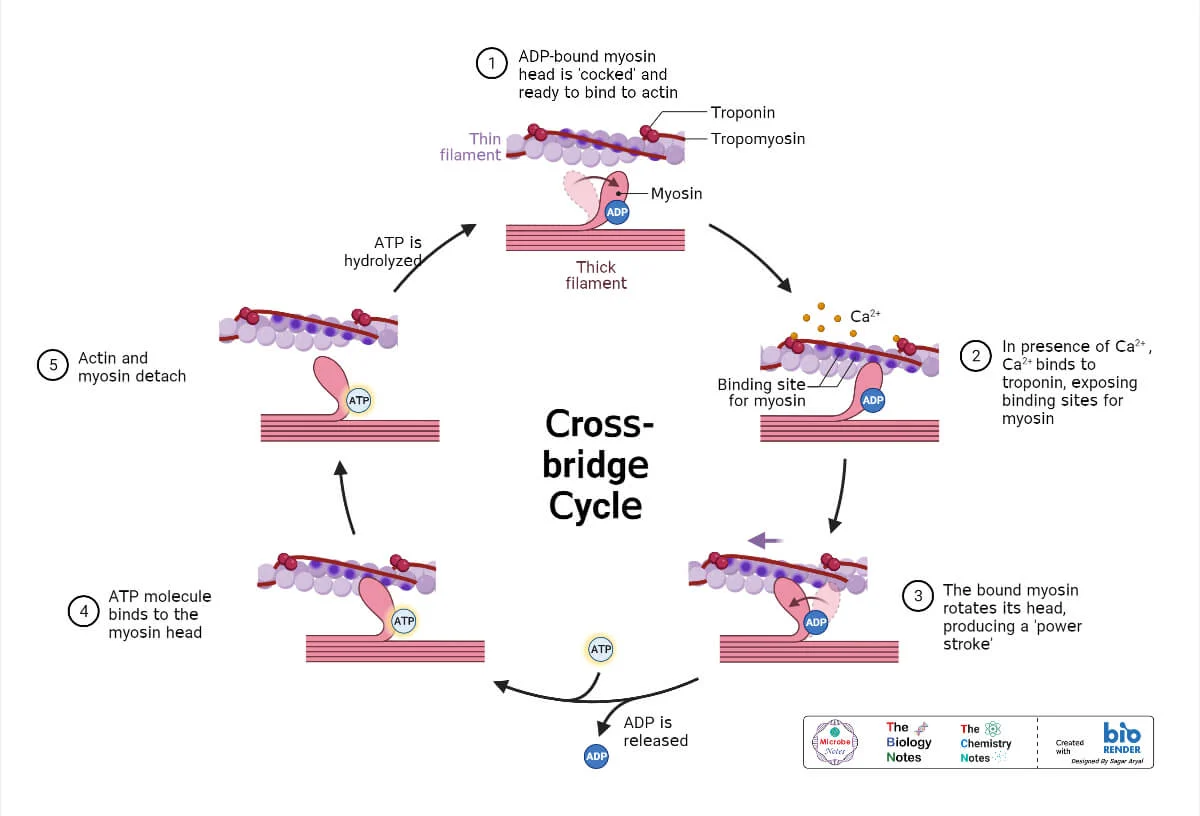
The cross-bridge cycle is a repetitive series of events that causes the thin filaments to slide over the thick filaments.
The energized ("cocked") myosin head, which is already holding onto ADP and inorganic phosphate (Pi) from the previous cycle, has a strong chemical attraction (affinity) for the actin filament. This binding can only occur if the myosin-binding sites on the actin are exposed. Once the sites are uncovered by the movement of tropomyosin (triggered by Ca²⁺ binding to troponin), the myosin head immediately forms a strong physical link with the actin. This connection is the "cross-bridge."
The formation of the cross-bridge triggers the release of the inorganic phosphate (Pi) from the myosin head. This release unleashes the stored energy, causing the myosin head to pivot forcefully from its high-energy 90° angle to a low-energy 45° angle. This pivotal movement is the power stroke. Because it is firmly attached, the myosin head drags the entire thin filament a short distance (~10 nm) toward the center of the sarcomere. Immediately after the pivot, the ADP molecule is also released, leaving the myosin head in a low-energy state, still tightly bound to actin.
After the power stroke, the myosin head is "stuck" to the actin in a low-energy state (the "rigor" state). The only way for it to let go is for a new molecule of ATP to bind to the ATP-binding site on the myosin head. This binding causes a conformational change that weakens the bond between myosin and actin, reducing their affinity for each other and causing the myosin head to detach. Without a fresh supply of ATP, this detachment cannot occur, which is the molecular basis for the muscle stiffness seen in rigor mortis after death.
The myosin head, now with ATP bound, immediately acts as an enzyme (myosin ATPase) and hydrolyzes the ATP back into ADP and inorganic phosphate (Pi). The energy released from breaking this ATP bond is captured by the myosin head and used to change its shape, moving it from its low-energy bent position back to its high-energy, upright, "cocked" position. It is now energized and reset, ready to begin the cycle again by binding to another active site further down the actin filament (if Ca²⁺ is still present).
Repeated cycles of the cross-bridge cycle cause:
When thousands of sarcomeres shorten simultaneously, the entire muscle shortens and generates force.
Muscle relaxation is an active, energy-requiring process.
A quiz covering Nerve and Muscle Physiology.
1. Which of the following is the primary role of the T-tubules in skeletal muscle contraction?
Correct (c): T-tubules conduct action potentials from the sarcolemma surface deep into the muscle fiber, ensuring simultaneous activation of all myofibrils.
Incorrect: Ca2+ storage is by the SR, ATP synthesis by mitochondria, and thin filament anchoring by Z-discs.
Analogy: Think of T-tubules as a subway system quickly delivering an important message (action potential) to all neighborhoods (myofibrils) within the muscle city.
2. Which ion's rapid influx into the motor neuron terminal triggers the release of acetylcholine (ACh)?
Correct (c): Influx of extracellular Ca2+ into the presynaptic terminal acts as the signal that triggers the fusion of ACh-containing vesicles with the presynaptic membrane.
Analogy: Ca2+ is like the "go-ahead" button for vesicles to release their neurotransmitter payload.
Incorrect: Na+ is for AP depolarization, K+ for repolarization, and Cl- for inhibition.
3. What is the primary function of acetylcholinesterase (AChE) at the neuromuscular junction?
Correct (c): AChE rapidly degrades ACh in the synaptic cleft, terminating the signal and allowing the muscle to relax and prepare for the next impulse.
Analogy: AChE is like a cleanup crew removing the "message" (ACh) from the bulletin board (receptor) promptly.
Incorrect: ACh synthesis and receptor binding are distinct processes; AChE's role is degradation.
4. The End-Plate Potential (EPP) at the neuromuscular junction is primarily caused by the net movement of which ions?
Correct (d): ACh opens non-selective cation channels. More Na+ rushes in than K+ leaves, causing a net influx of positive charge and depolarization (EPP).
Incorrect: The directions of ion movement are wrong or the primary ion is incorrect.
5. What is the direct consequence of Ca2+ binding to Troponin C in skeletal muscle?
Correct (b): Ca2+ binding to Troponin C causes a conformational change that pulls tropomyosin away from the myosin-binding sites on actin, allowing cross-bridge formation.
Analogy: Ca2+ is like a key that unlocks a protective shield (tropomyosin) covering the active sites.
Incorrect: ATP binding causes detachment; ATP hydrolysis cocks the myosin; Ca2+ reuptake occurs during relaxation.
6. During the power stroke, which event immediately follows the binding of the myosin head to actin?
Correct (b): The sequence is: energized myosin (ADP+Pi) binds actin -> Pi is released -> Power stroke (ADP released) -> ATP binds causing detachment.
Incorrect: ATP binding causes detachment, Pi release triggers the power stroke, and Ca2+ reuptake is for relaxation.
7. Which component of the sarcomere remains unchanged in length during muscle contraction?
Correct (c): The A band corresponds to the length of the thick filament, which does not shorten; thin filaments slide over it.
Incorrect: I band, H zone, and sarcomere length all shorten during contraction.
8. Which statement about the role of ATP in muscle contraction is TRUE?
Correct (b): A new ATP molecule must bind to the myosin head to reduce its affinity for actin, allowing detachment.
Incorrect: Ca2+ moves tropomyosin; ATP hydrolysis energizes myosin for the power stroke after binding; ATP is crucial for both contraction and relaxation.
9. What is the primary role of voltage-gated Ca2+ channels in the motor neuron terminal?
Correct (c): When the action potential arrives, it opens these channels, allowing Ca2+ influx which signals synaptic vesicles to release ACh.
Incorrect: Action potentials are initiated by Na+ channels; repolarization by K+ channels; EPPs are on the muscle fiber.
10. Blocking Ryanodine Receptors (RyRs) on the SR would directly prevent:
Correct (c): RyRs are the Ca2+ release channels on the SR. Blocking them prevents Ca2+ from escaping the SR into the sarcoplasm, thus halting contraction.
Incorrect: ACh release is presynaptic; muscle APs are on the sarcolemma; Ca2+ reuptake is by SERCA pumps.
11. Why is the action potential in a motor neuron considered "all-or-nothing"?
Correct (b): If the threshold is reached, a full-sized action potential occurs; if not, none occurs. Its amplitude is constant, independent of stimulus strength beyond threshold.
Analogy: It's like flushing a toilet – you either push the handle enough to flush completely, or nothing happens. There's no "half-flush."
12. During muscle relaxation, what happens to Ca2+ in the sarcoplasm?
Correct (b): Relaxation requires active pumping of Ca2+ back into the SR by SERCA pumps, which lowers sarcoplasmic Ca2+ levels.
Incorrect: Ca2+ detaches from troponin when its concentration drops; it doesn't diffuse out of the cell; RyRs are closed by low Ca2+ (indirectly).
13. Which component of the thin filament directly binds to Ca2+ ions to initiate contraction?
Correct (d): Troponin C (TnC) is the specific subunit of the troponin complex that binds Ca2+ ions, initiating the conformational change leading to contraction.
Incorrect: Actin has myosin-binding sites; tropomyosin blocks them; TnT binds tropomyosin.
14. What happens to ADP and Pi immediately prior to the power stroke?
Correct (c): After the energized myosin head (with ADP + Pi) binds to actin, Pi is released, triggering the power stroke. ADP is released during the power stroke itself.
15. If a motor neuron's action potential fails to reach the presynaptic terminal, what is the direct consequence?
Correct (c): The action potential reaching the presynaptic terminal is the critical trigger for Ca2+ influx and subsequent ACh release. Without it, the NMJ process fails.
Incorrect: Without the AP, there's no release, controlled or uncontrolled. Receptor sensitivity isn't directly altered. Ca2+ reuptake is for relaxation, not relevant here.
16. The specialized endoplasmic reticulum that stores and releases Ca2+ ions in a muscle fiber is called the ____________________.
17. The functional contractile unit of a myofibril, extending from one Z-disc to the next, is the _________.
18. The release of _________ from the motor neuron terminal initiates the process at the neuromuscular junction.
19. During the cross-bridge cycle, the binding of new ATP to myosin causes it to _________ from actin.
20. DHPRs in T-tubules are mechanically linked to _________ on the SR, which act as Ca2+ release channels.
Your Score:
0%
0 / 0 correct
Excitability: The Ability to Respond and Communicate
Excitability refers to the ability of a cell to respond to a stimulus by generating an electrical signal called an action potential. It can be defined as a physical chemical change that occurs when a stimulus is applied on a tissue. A stimulus is an external agent that produces excitation in a tissue. This electrical signal is then propagated along the cell membrane or transmitted to other cells, leading to a specific physiological response.
The action potential is a transient, rapid, and self-propagating reversal of the electrical potential across the cell membrane. This electrical signal is the medium through which cells rapidly transmit information, either along the length of an individual cell or to other cells via specialized junctions. This property is crucial for rapid communication and coordination within the body, underpinning virtually every complex physiological function, from perception and thought to movement and visceral regulation.
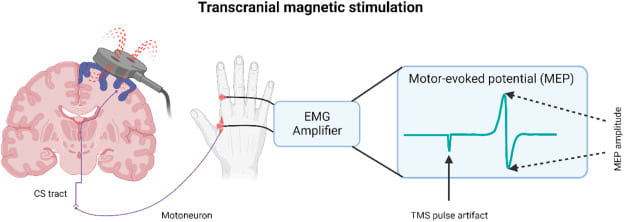
Think of an excitable cell like a highly sensitive electrical tripwire or alarm system. The resting state is the armed system waiting for a trigger. The stimulus is the pressure that activates the tripwire. The action potential is the immediate, swift, and uniform "alarm bell" that rings loudly and clearly, sending its message through the system to orchestrate a coordinated response.
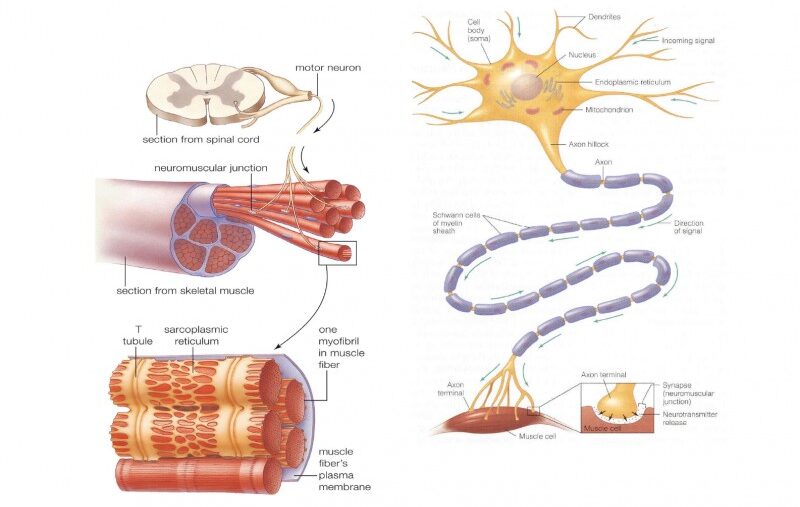
While all living cells exhibit some degree of responsiveness, only a select group possess the highly specialized machinery to generate and propagate rapid electrical signals. These are the "excitable cells."
Expanded Role: Neurons are the fundamental units of the nervous system. Their primary function is the transmission of electrical and chemical signals for sensory input, integration, motor output, cognition, and emotion.
Unique Features: They possess specialized structures like dendrites (to receive signals), a cell body (soma), and a long axon (to transmit signals), often insulated by a myelin sheath to speed conduction.
Muscle cells are specialized for contraction, which generates force and movement. Their excitability is the prerequisite for this mechanical action.
Responsible for all voluntary movements (walking, speaking, breathing). When a motor neuron sends an action potential, it triggers a muscle action potential, leading to contraction.
Found only in the heart, responsible for the rhythmic and involuntary pumping of blood. They possess autorhythmicity and have distinctively long action potentials for coordinated contractions.
Mediate involuntary movements in the walls of internal organs like the digestive tract, blood vessels, and urinary bladder. Their excitability is influenced by stretch, local chemicals, and the autonomic nervous system.
Role Expansion: Many glandular cells (e.g., in the adrenal medulla, pancreas) exhibit excitability. They can respond to an electrical stimulus from a neuron by generating their own electrical event (depolarization or action potential).
Excitability Link: This electrical event is typically coupled to the release of their secretions (e.g., hormones, digestive enzymes). For example, adrenal medullary cells depolarize in response to a neuronal signal, triggering Ca²⁺ influx and the exocytosis of epinephrine. This ensures precise and rapid control over hormone release.
The capacity of these cells to generate electrical signals rests entirely on the idea of membrane potential.
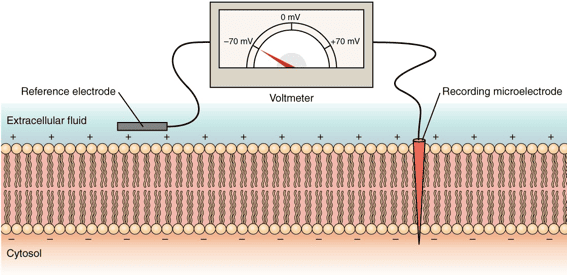
This is the voltage difference across the cell's outer boundary, a stored electrical energy created by an uneven distribution of ions (electrically charged particles) inside the cell (ICF) and outside the cell (ECF).
When an excitable cell is quiet, it maintains a stable, baseline electrical charge called the Resting Membrane Potential (RMP). In this state, the inside of the cell consistently holds a negative charge relative to the outside (e.g., -70 mV in neurons, -90 mV in skeletal muscle).
The RMP is a dynamic state, constantly maintained by an interplay of three factors:
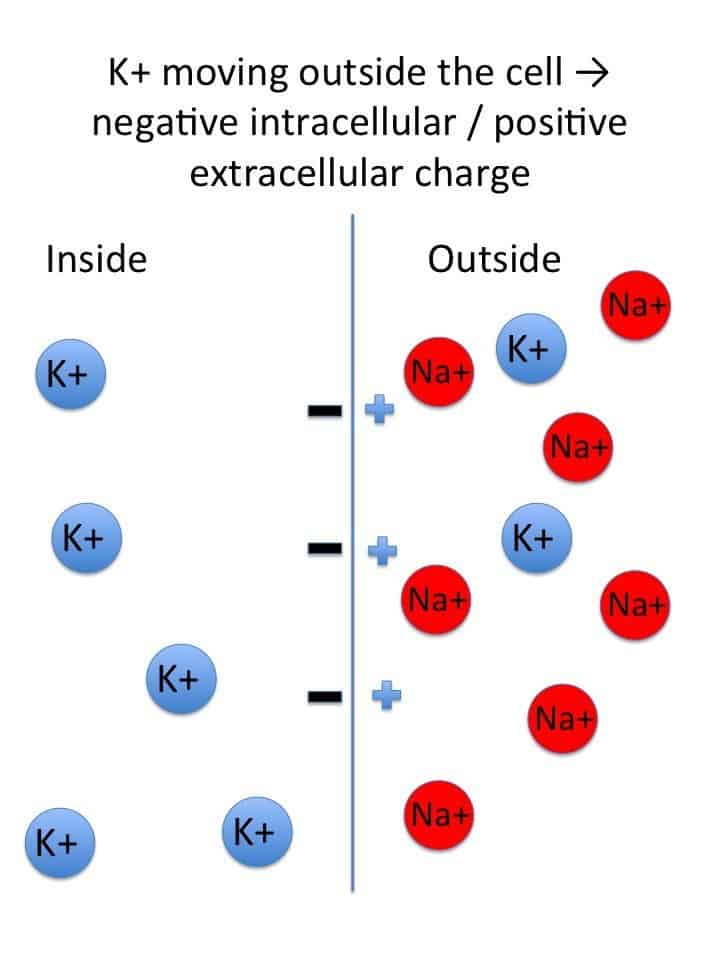
The equilibrium potential for a specific ion is the membrane voltage at which there is no net movement of that ion across the membrane. At this voltage, the electrical force is perfectly balanced by the chemical (concentration) force. The Nernst Equation calculates this value:
E_ion = (RT / zF) * ln([ion]out / [ion]in)
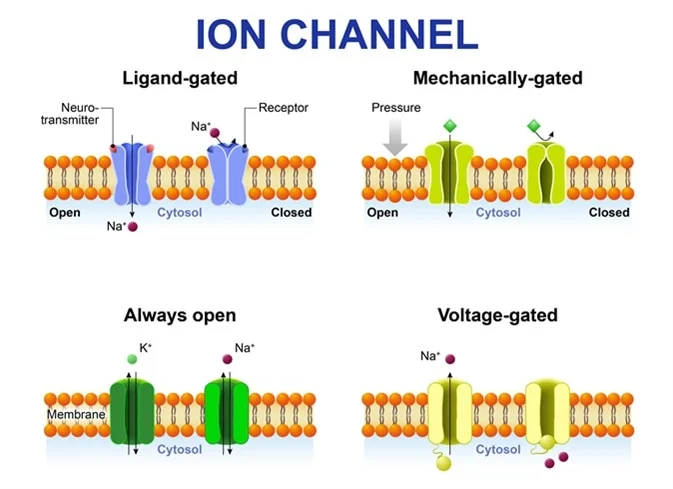
These are specialized proteins that form pores for specific ions to cross the membrane.
These channels open or close only in response to a particular trigger and are essential for generating action potentials.
Open or close in direct response to changes in membrane voltage. They are the key drivers of the action potential.
Open or close when a specific chemical messenger (a ligand), such as a neurotransmitter, binds to them.
Open or close when they are physically deformed or stretched, critical for sensory perception like touch and pressure.
A stimulus is any detectable change (electrical, chemical, or mechanical) in the cell's environment that has the potential to alter its RMP.
Threshold is the crucial voltage level that depolarization must reach for an action potential to fire (typically around -55 mV in neurons). It is an "all-or-none" event: if a stimulus causes a depolarization that reaches threshold, a full action potential fires. If it does not, nothing happens.
The action potential is the primary electrical signal employed by excitable cells to swiftly transmit information across significant distances. It stands as an "all-or-nothing" phenomenon: once initiated, it proceeds through its entire sequence with consistent strength, never diminishing.
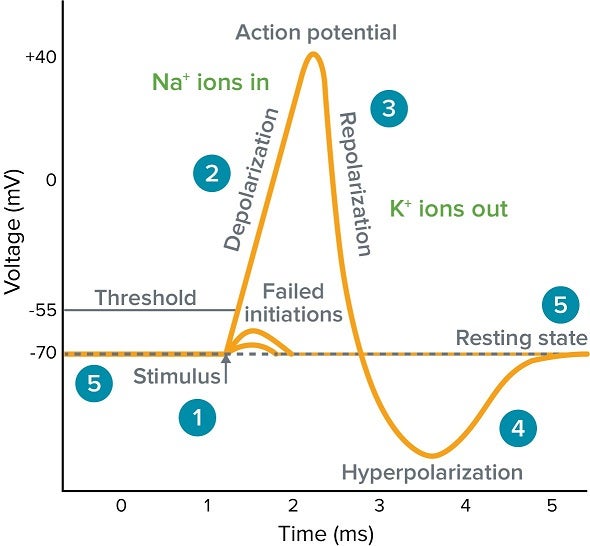
All voltage-gated Na⁺ and K⁺ channels are closed. The RMP is maintained by K⁺ leak channels and the Na⁺/K⁺ pump.
A local stimulus causes a few voltage-gated Na⁺ channels to open, allowing a small amount of Na⁺ to enter. If enough Na⁺ enters to raise the membrane potential to the threshold level, an action potential is triggered.
Once threshold is reached, a vast number of voltage-gated Na⁺ channels open very rapidly. A massive and swift surge of Na⁺ into the cell causes the inside of the membrane to become positive.
At the peak, the voltage-gated Na⁺ channels inactivate (their inactivation gates close), stopping Na⁺ influx. Simultaneously, the slower voltage-gated K⁺ channels are now fully open, allowing a significant outflow of K⁺, which rapidly restores the membrane's negative charge.
The voltage-gated K⁺ channels close slowly, allowing K⁺ to continue exiting for a brief period. This causes the membrane to become temporarily more negative than the RMP.
The slow K⁺ channels finally close, and the ever-active Na⁺/K⁺ pump helps to re-establish the original ion concentration gradients, returning the membrane to its stable RMP.
The electrical shift at one point on the membrane triggers the opening of voltage-gated Na⁺ channels in the immediately adjacent area. This process repeats, moving the signal along the length of the nerve or muscle fiber.
Many nerve fibers are insulated by a fatty myelin sheath. Action potentials therefore appear to "jump" from one uninsulated gap (a node of Ranvier) to the next. This rapid "jumping" process is termed saltatory conduction and dramatically increases the signal's speed.
Just as cells must generate signals, they also need ways to inhibit them, ensuring precise control and preventing uncontrolled firing.
Inhibitory neurotransmitters (like GABA or glycine) open ion channels that either allow Cl⁻ to enter the cell or K⁺ to leave. The outcome is an increase in the negative charge inside the cell (e.g., from -70 mV to -75 mV), making it significantly harder for the cell to reach the threshold and fire an action potential.
An inhibitory neuron releases neurotransmitter (e.g., GABA) directly onto the axon terminal of an excitatory neuron. This reduces the electrical charge of the terminal, so when an action potential arrives, fewer excitatory neurotransmitters are released. This allows for fine-tuning and selective reduction of specific signals.
A vast array of drugs and toxins work by directly interfering with ion channels.
An in-depth comprehension of cellular excitability is absolutely vital for understanding, diagnosing, and creating effective treatments for numerous conditions affecting the nervous system and muscles.
The precise balance of ions is paramount for proper excitability.
Hyperkalemia (Elevated K⁺)High extracellular K⁺ makes the resting membrane potential less negative (closer to threshold). While this might initially increase excitability, prolonged depolarization can inactivate voltage-gated Na⁺ channels, rendering cells inexcitable. This is life-threatening for heart muscle cells and can lead to cardiac arrest.
Hypokalemia (Low K⁺)Low extracellular K⁺ makes the resting membrane potential more negative (hyperpolarized). This moves the cell further from threshold, making it less excitable and leading to symptoms like muscle weakness and dangerous heart arrhythmias.
Sodium Imbalances (Hypernatremia/Hyponatremia)Since the influx of Na⁺ is the primary driver of depolarization, imbalances in Na⁺ levels can significantly impair the ability of nerve and muscle cells to generate action potentials.
Calcium ImbalancesAn Excitability Exam covering core neurophysiology concepts.
1. Which ion is primarily responsible for the rapid depolarization (rising phase) of a typical neuronal action potential?
Correct (c): The rapid influx of positively charged Na+ ions through voltage-gated Na+ channels causes the membrane potential to swiftly become positive during the rising phase.
Incorrect: K+ is for repolarization, Cl- for inhibition, and Ca2+ for neurotransmitter release.
Analogy: Think of Na+ as the "gas pedal" for the action potential. Pushing it hard (opening Na+ channels) makes the electrical signal quickly accelerate upwards.
2. The Resting Membrane Potential (RMP) is primarily maintained by which two factors?
Correct (c): The RMP is established by the Na+/K+-ATPase pump (which creates the gradients) and the high permeability of the membrane to K+ ions through K+ leak channels (allowing K+ to slowly exit).
Incorrect: Voltage-gated and ligand-gated channels are primarily involved in generating signals (action potentials, synaptic potentials), not maintaining the baseline RMP.
3. What event immediately follows the membrane potential reaching threshold?
Correct (b): Reaching threshold triggers a massive opening of voltage-gated Na+ channels, leading to a huge Na+ influx and the rapid depolarization. This is a positive feedback loop.
Incorrect (a): K+ channels open slowly and are for repolarization.
Analogy: Reaching threshold is like the first domino falling, triggering a chain reaction where all the other dominoes (voltage-gated Na+ channels) quickly topple over.
4. The absolute refractory period of an action potential is primarily caused by:
Correct (b): During this period, the voltage-gated Na+ channels are in an inactivated state and cannot open again, regardless of stimulus strength, preventing another action potential.
Incorrect (a): Slow closing of K+ channels contributes to the relative refractory period.
Analogy: The inactivation gate of the Na+ channel is like a "do not disturb" sign. Once it's up, no matter how hard you knock, you can't start another action potential until it's taken down.
5. Myelination of an axon primarily serves to:
Correct (d): Myelin acts as an electrical insulator, forcing the action potential to "jump" between nodes of Ranvier (saltatory conduction), which significantly speeds up signal transmission.
Incorrect (a): Action potential amplitude is "all-or-nothing."
Incorrect (c): The refractory period ensures unidirectional propagation.
6. Which condition would make a cell less excitable by hyperpolarizing its RMP?
Correct (c): If negative Cl- ions enter the cell, they make the inside more negative, driving the membrane potential further away from the threshold, thus reducing excitability.
Incorrect (a): Opening Na+ channels causes depolarization, making it more excitable.
7. In the context of action potentials, "all-or-nothing" means:
Correct (c): If a stimulus is strong enough to reach threshold, a full-sized action potential occurs. If it's below threshold, no action potential occurs. The size of the AP is independent of stimulus strength.
Analogy: It's like flipping a light switch. You either press it hard enough to turn the light completely ON, or it stays OFF. There's no "half-on" setting.
8. Which phase is characterized by K+ outflow and Na+ channel inactivation?
Correct (d): During repolarization, voltage-gated Na+ channels inactivate (stop Na+ influx), and voltage-gated K+ channels are fully open, allowing K+ to exit the cell, bringing the membrane potential back down.
9. A drug that blocks voltage-gated Na+ channels would primarily affect:
Correct (b): Voltage-gated Na+ channels are essential for the rapid depolarization phase. Blocking them prevents the action potential from initiating and propagating.
Analogy: Blocking Na+ channels is like taking the ignition key out of a car. You can't start the engine (action potential) at all.
10. Which of the following best describes Multiple Sclerosis (MS)?
Correct (b): MS is characterized by the destruction of the myelin sheath that insulates axons, which directly disrupts the efficient and rapid propagation of action potentials.
Incorrect (a): This describes epilepsy.
Incorrect (c): This describes Myasthenia Gravis.
11. The Equilibrium Potential for an ion is the membrane potential where:
Correct (b): At the equilibrium potential, the electrical force pulling the ion is exactly equal and opposite to the chemical (concentration) force pushing it, resulting in no net movement.
12. Presynaptic inhibition reduces an excitatory signal by:
Correct (c): Presynaptic inhibition involves an inhibitory neuron acting on the axon terminal of an excitatory neuron, reducing the amount of neurotransmitter released when an action potential arrives.
Incorrect (a): This would be postsynaptic inhibition.
13. A patient with hypokalemia (low extracellular K+) would likely experience:
Correct (b): With less K+ outside, the K+ gradient out of the cell becomes steeper, causing more K+ to leave. This makes the inside more negative (hyperpolarized), moving the RMP further from threshold and making cells less excitable.
14. What is the role of the inactivation gate of the voltage-gated Na+ channel?
Correct (c): The inactivation gate closes a few milliseconds after the activation gate opens, stopping Na+ influx. This is essential for repolarization and prevents immediate re-firing (absolute refractory period).
Incorrect (a): This is the role of the activation gate.
15. Which ion's movement is primarily responsible for the "afterhyperpolarization" (undershoot) phase?
Correct (b): Afterhyperpolarization occurs because voltage-gated K+ channels are slow to close, allowing K+ to continue exiting the cell for a short period, making the membrane temporarily more negative than RMP.
16. The critical electrical level that must be reached for an action potential to be generated is known as the _________ potential.
17. Local anesthetics like Lidocaine work by blocking voltage-gated _________ channels.
18. In Multiple Sclerosis, the loss of the myelin sheath leads to impaired action potential _________.
19. The period when a second AP cannot be generated, regardless of stimulus strength, is the _________ refractory period.
20. Neurotransmitters like GABA and glycine can inhibit excitability by causing the influx of _________ ions.
Your Score:
0%
0 / 0 correct
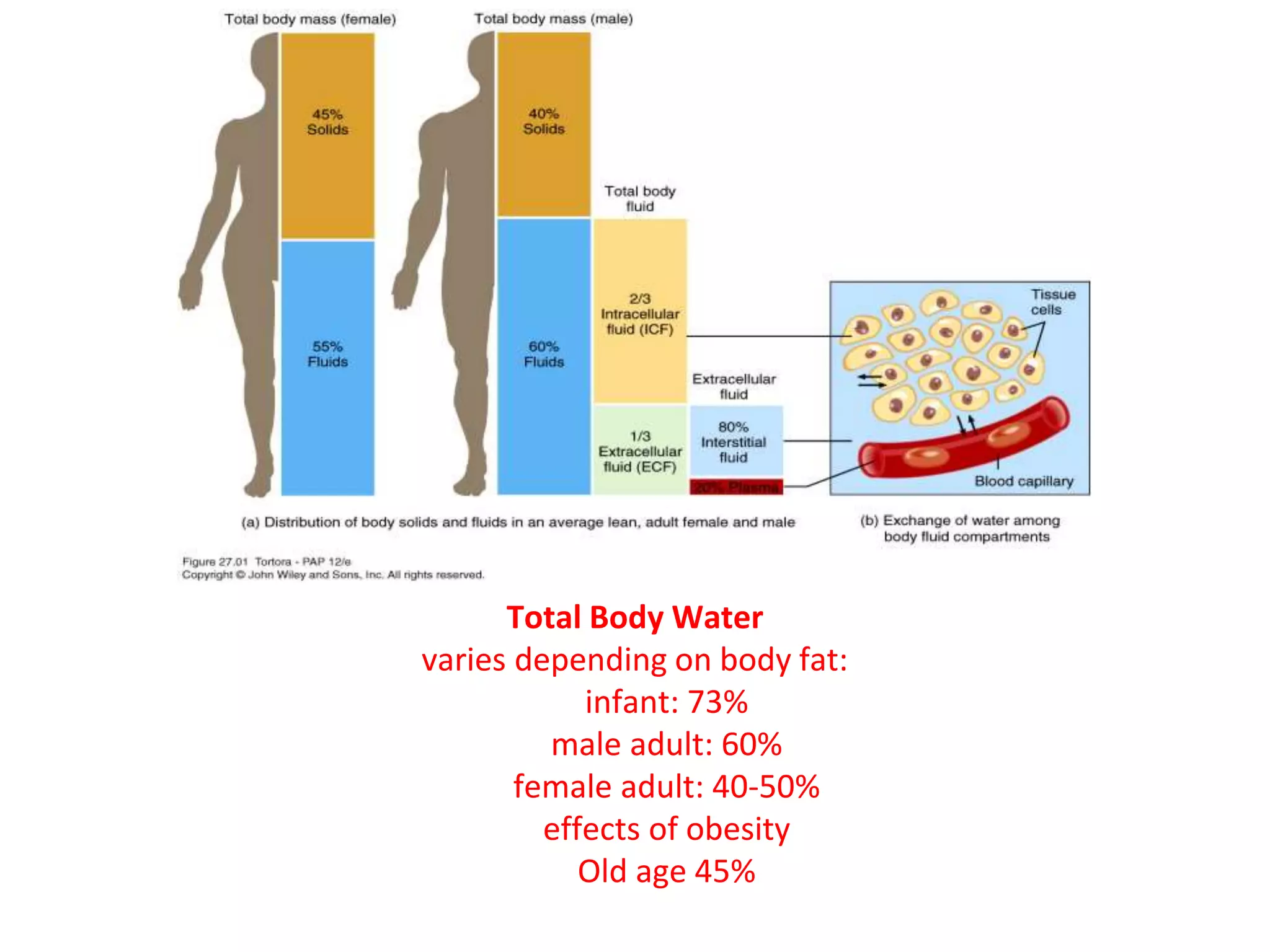
To truly appreciate the dynamics of body fluids, we first need to understand where all this fluid is located within the body. Imagine your body as a system of interconnected containers, each holding a specific type of fluid. These "containers" are what we call body fluid compartments.
The human body is largely composed of water, and this water isn't just free-flowing; it's meticulously organized into various functional compartments. This compartmentalization is key to maintaining cellular and systemic homeostasis.
TBW refers to all the water contained within the body. It represents a significant proportion of body mass.
Approximately 60% of an adult's body weight is water. This percentage can vary significantly based on several factors:
TBW is not pure water; it contains numerous dissolved solutes, including electrolytes, proteins, nutrients, gases, and waste products. The total amount of water in an adult human body constitutes about 50-70% of the total body weight. This water is not uniformly distributed but is divided into two primary compartments, which are further subdivided:
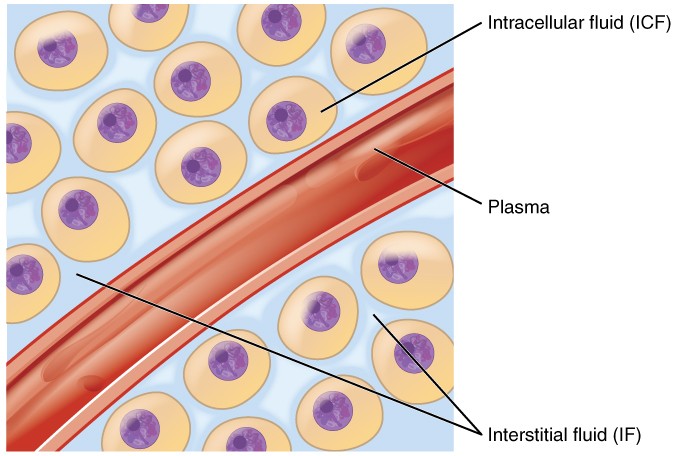
Location: The ICF is the fluid found within the cells of the body. It is the immediate environment where the vast majority of cellular metabolic activities take place.
Proportion and Significance: The ICF constitutes the largest single fluid compartment, accounting for approximately two-thirds (2/3) of the Total Body Water (TBW). In an adult male weighing 70 kg, this would be roughly 28 liters (40% of body weight). This large volume underscores its critical role: it directly bathes the cellular machinery, providing the aqueous medium for all intracellular biochemical reactions.
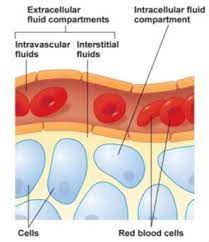
Location: The ECF is all the fluid found outside the cells. It acts as the body's internal environment that bathes all cells.
Proportion: The ECF constitutes approximately one-third (1/3) of the TBW, which is roughly 14 liters (20% of body weight) in a 70 kg adult.
The ECF is not a monolithic entity; it is further subdivided into several distinct yet interconnected compartments:
This is the "tissue fluid," filling the microscopic spaces between the cells. It is the largest component of the ECF, comprising about 80% of ECF volume. Its ionic composition is similar to plasma, but it has a significantly lower protein concentration. The ISF is the critical medium for the exchange of nutrients, gases, and waste between the blood and the cells.
This is the fluid component of blood, circulating within the cardiovascular system. It accounts for about 20% of ECF volume. Its defining characteristic is its high concentration of plasma proteins (e.g., albumin). Plasma is the primary transport medium for blood cells, nutrients, hormones, and waste products.
A small, specialized component of the ECF, representing only 1-2% of body weight. It consists of fluids secreted by specific cells into distinct, epithelial-lined spaces. The composition of these fluids is often unique and tailored to their specific function.
Examples: Cerebrospinal Fluid (CSF), Intraocular Fluid, Synovial Fluid, Serous Fluids (pleural, pericardial), and Gastrointestinal Secretions.
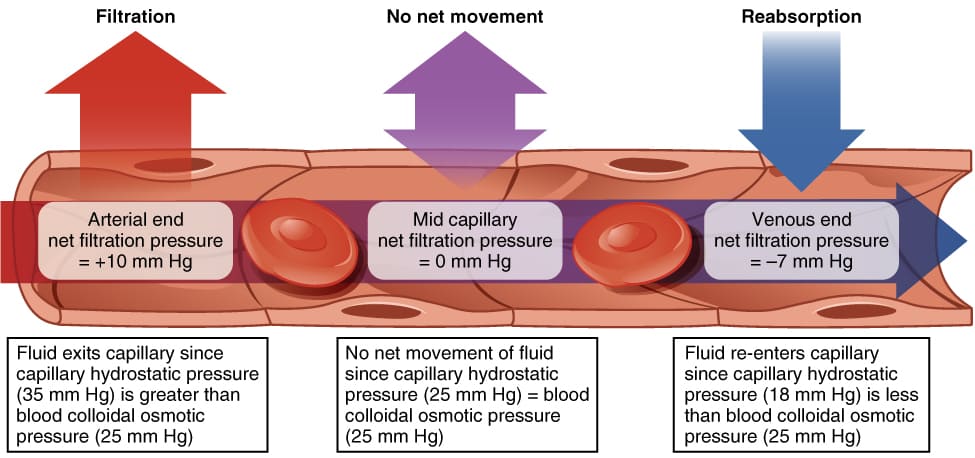
The precise movement of water and solutes between the body's fluid compartments is a cornerstone of physiological homeostasis. This dynamic equilibrium is meticulously regulated by physical forces, membrane properties, and complex neurohormonal systems.
The exchange of fluid, nutrients, gases, and waste products between the blood (plasma) and the cells (via the ISF) occurs primarily across the thin walls of the capillaries. This movement is governed by Starling Forces, which represent the interplay of hydrostatic and oncotic pressures.
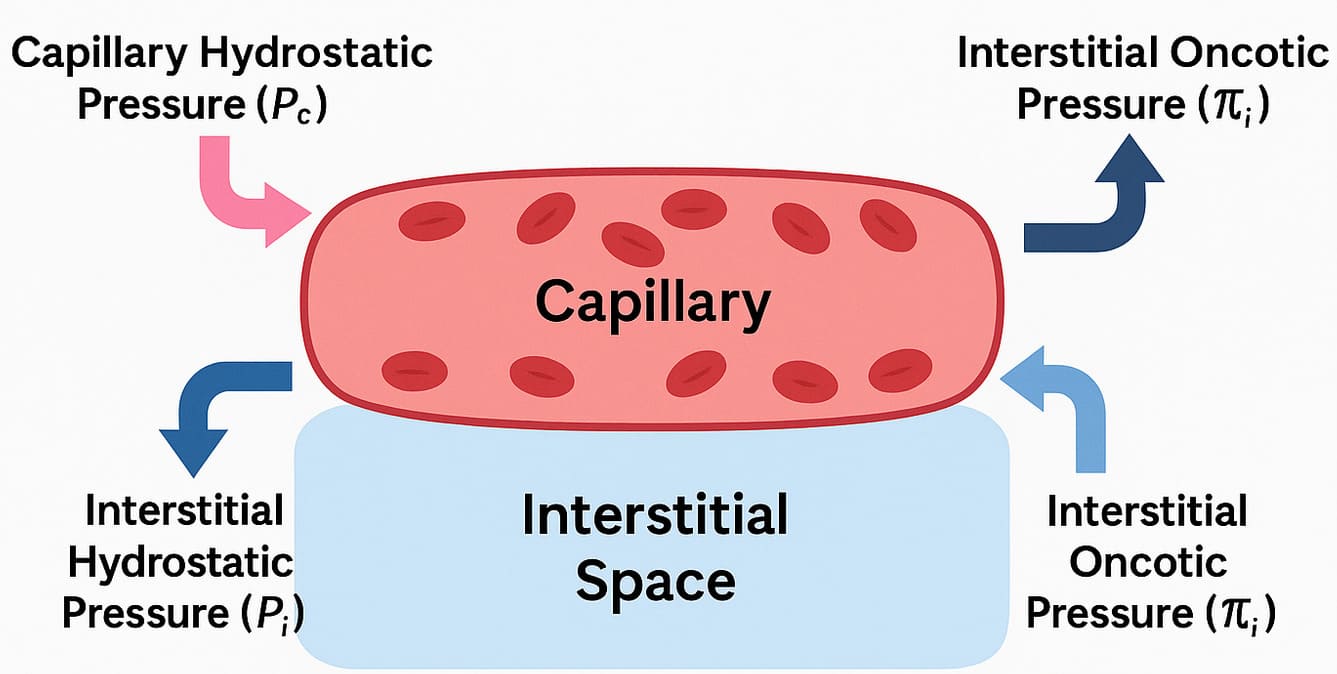 Starling Forces - The Drivers of Capillary Exchange:
Starling Forces - The Drivers of Capillary Exchange:The net movement of fluid is determined by the balance of these forces, expressed by the Starling equation: NFP = (Pc - Pif) - (πc - πif)
There is a slight imbalance where filtration slightly exceeds reabsorption. This excess fluid and any leaked proteins are collected by the lymphatic system, which acts as a drainage system, returning this "lymph" to the circulation. This is vital for preventing interstitial edema. Failure of this system results in lymphedema.
The exchange between the ISF and the ICF is driven primarily by osmosis. The cell membrane is highly permeable to water (largely via aquaporins) but relatively impermeable to most solutes.
Tonicity describes the effect a solution has on cell volume, based on its concentration of non-penetrating solutes.
While water movement is passive, the maintenance of the osmotic gradients is dependent on active transport. The Na⁺/K⁺ ATPase pump is critical. By constantly pumping 3 Na⁺ out and 2 K⁺ in, it counters the natural tendency of water to enter the cell (due to the high concentration of trapped intracellular proteins), thereby maintaining cell volume and preventing lysis.
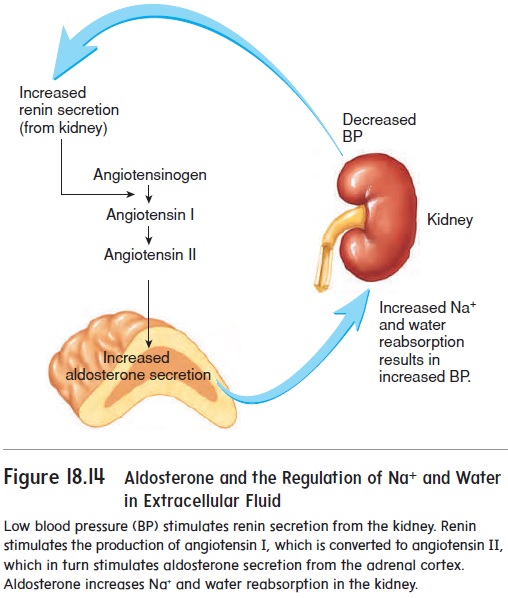
This is achieved through complex, interconnected neurohormonal feedback systems.
ECF volume is primarily determined by its sodium content, as "where Na⁺ goes, water follows."
ECF osmolarity is primarily determined by the concentration of solutes relative to water, and is tightly controlled to stay within 280-300 mOsm/L.
Disturbances in fluid regulation can have profound and life-threatening consequences.
The volume of a compartment is calculated as: Volume = Mass of Indicator Injected / Concentration of Indicator in Sample. The key is choosing an indicator that distributes only in the target compartment.
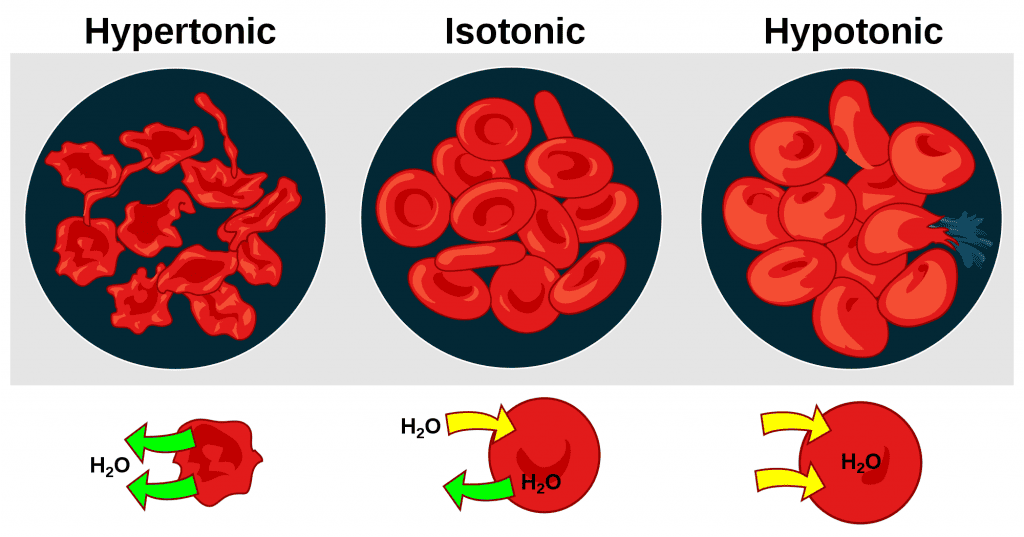
The human body is an intricate system highly dependent on the precise balance of water and solutes across its various compartments. Understanding the concepts of osmolarity and tonicity, and their clinical implications, particularly with intravenous (IV) fluid administration, is fundamental to effective medical practice.
These two terms are often used interchangeably, but they possess distinct physiological meanings that are critical when considering fluid shifts across cell membranes.
A solution can be isosmotic but hypotonic. A classic example is 5% Dextrose in Water (D5W). Initially, its osmolarity is ~252 mOsm/L (isosmotic). However, once cells metabolize the glucose, it leaves behind pure water, which is hypotonic to cells, causing water to shift into them. Therefore, tonicity, not just osmolarity, is what truly matters for predicting cell volume changes.
Their safe and effective administration requires a deep understanding of their tonicity and how they distribute.
Products like packed red blood cells (PRBCs) are considered isotonic. Their distribution primarily expands the intravascular compartment (plasma volume) and directly increases the oxygen-carrying capacity of the blood.
| IV Fluid Type | Tonicity | Final Distribution | Effect on Cells | Primary Clinical Use |
|---|---|---|---|---|
| Isotonic | Isotonic | Expands ECF (Plasma + ISF) | No change | ECF volume expansion (shock, dehydration) |
| Hypotonic | Hypotonic | Shifts from ECF to ICF | Swell | Cellular rehydration (hypernatremia) |
| Hypertonic | Hypertonic | Shifts from ICF to ECF | Shrink | Reduce cerebral edema, treat severe hyponatremia |
| Colloids | Isotonic | Primarily remains in Plasma | No change | Plasma volume expansion (severe shock) |
| Blood Products | Isotonic | Primarily remains in Plasma | No change | Replace blood loss, improve O₂ carrying capacity |
At the heart of all physiological processes involving fluids is the interaction between solutes and solvents, and their movement across various compartments.
The primary and overwhelmingly abundant solvent in all body fluids is WATER (H₂O).
Water's unique properties make it an ideal biological solvent:
Body fluids are complex solutions containing a vast array of solutes:
The movement of substances is primarily governed by passive processes that do not require cellular energy (ATP).
These passive movements are essential for:
Basic Principle: Water follows solutes. Specifically, water moves from an area of lower effective solute concentration (higher water concentration) to an area of higher effective solute concentration (lower water concentration) across a semipermeable membrane.
| IV Fluid Type | Effective Tonicity | Primary Distribution | Effect on ICF Cells |
|---|---|---|---|
| Isotonic (NS, LR) | Isotonic | ECF only (plasma & ISF) | No change |
| Hypotonic (0.45% NaCl, D5W) | Hypotonic | ECF & ICF | Swell |
| Hypertonic (3% NaCl) | Hypertonic | ECF (draws from ICF) | Shrink |
| Colloids (Albumin) | Effectively Hypertonic (oncotic) | Plasma only (draws from ISF) | No direct effect |
A quiz on Body Fluids, Osmolarity, Tonicity & IV Solutions.
1. Which of the following best defines osmolarity?
Correct (c): Osmolarity measures the sum of all solute particles, both penetrating (ineffective) and non-penetrating (effective), in a given volume of solution.
Incorrect (a, b): This defines tonicity.
Incorrect (d): This describes osmotic pressure.
2. A solution with a lower concentration of non-penetrating solutes than the cell's cytoplasm is described as:
Correct (c): Hypotonic solutions have fewer non-penetrating solutes, causing water to move into cells and make them swell.
Incorrect (b): Isotonic solutions have the same concentration, causing no change in cell volume.
Incorrect (d): Hypertonic solutions have a higher concentration, causing cells to shrink.
3. Which solute is generally considered an ineffective osmole in the context of sustained osmotic gradients across cell membranes?
Correct (c): Urea readily crosses most cell membranes, so it does not create a sustained osmotic gradient and is an ineffective osmole.
Incorrect (a): Sodium is the primary effective osmole in the ECF.
Incorrect (d): Mannitol is specifically designed not to cross membranes, making it a potent effective osmole.
4. Normal plasma osmolarity is approximately:
Correct (b): This is the tightly regulated normal range for plasma osmolarity in humans.
Incorrect: The other ranges are either too low or too high for a healthy state.
5. When a cell is placed in a hypertonic solution, what will happen to the cell?
Correct (c): In a hypertonic solution, the ECF has more non-penetrating solutes, pulling water out of the cell via osmosis and causing it to shrink.
Incorrect (a): This happens in a hypotonic solution.
Incorrect (b): This happens in an isotonic solution.
Incorrect (d): Water moves passively by osmosis.
6. A patient with severe hypovolemic shock requires rapid fluid resuscitation. Which IV fluid is most appropriate?
Correct (d): Isotonic crystalloids like Lactated Ringer's are first-line for hypovolemic shock because they expand the extracellular fluid volume without causing dangerous fluid shifts.
Incorrect (a, b): These are hypotonic and would shift water into cells, worsening intravascular depletion.
Incorrect (c): This is hypertonic and used for specific conditions like cerebral edema, not routine resuscitation.
7. How does 5% Dextrose in Water (D5W) behave clinically after the glucose is metabolized?
Correct (c): Once the glucose is metabolized, it leaves behind pure water. This "free water" then moves into cells due to osmosis, effectively acting as a hypotonic solution and rehydrating cells.
8. What is a primary clinical indication for administering a hypertonic saline solution (e.g., 3% NaCl)?
Correct (b): Hypertonic saline is used to rapidly raise ECF sodium and pull water out of swollen brain cells in life-threatening hyponatremia.
Incorrect (a): Hypernatremia is treated with hypotonic solutions.
Incorrect (c): It is a high-risk fluid, not for routine use.
9. What is the main advantage of colloids over crystalloids for plasma volume expansion?
Correct (c): Due to their large molecules remaining in the intravascular space and exerting oncotic pressure, colloids expand plasma volume with a smaller amount of fluid compared to crystalloids.
Incorrect (a): Colloids are significantly more expensive.
Incorrect (b): Crystalloids distribute throughout the ECF; colloids largely stay in the plasma.
10. The primary solvent in all human body fluids is:
Correct (c): Water is the universal solvent for biological systems, making up the vast majority of all body fluids.
Incorrect: The other options are important solutes, not the solvent.
11. The net movement of solute particles from an area of higher to lower concentration is called:
Correct (c): Diffusion is the passive movement of solute particles down their concentration gradient.
Incorrect (a): Osmosis is the movement of water (the solvent).
Incorrect (b): Active transport requires energy to move solutes against a gradient.
12. Which type of diffusion requires membrane proteins but not ATP?
Correct (b): Facilitated diffusion uses membrane proteins (channels or carriers) to help solutes move down their gradient, without ATP.
Incorrect (a): Simple diffusion does not require proteins.
Incorrect (c): Active transport requires ATP.
13. A patient with severe hypernatremia would most likely benefit from which type of IV fluid?
Correct (c): In hypernatremia, the ECF is hypertonic, causing cells to shrink. A hypotonic solution will dilute the ECF sodium and cause water to move back into the cells, rehydrating them.
14. What is the approximate distribution of 1 liter of an isotonic crystalloid (like Normal Saline) after infusion?
Correct (c): Isotonic crystalloids distribute throughout the entire ECF. Since the ECF is roughly 1/4 plasma and 3/4 interstitial fluid, an infused liter will partition accordingly.
15. Why are brain cells particularly vulnerable to rapid shifts in ECF osmolarity?
Correct (b): The brain's enclosure within the skull means that significant swelling (from hypotonicity) or shrinking (from hypertonicity) can lead to severe neurological damage.
16. The term describing the effect a solution has on cell volume is _________.
17. In osmosis, water moves toward an area of _________ solute concentration.
18. _________ are solutions with large molecules that primarily remain within the intravascular compartment.
19. The primary cation in the ECF that is a major effective osmole is _________.
20. When a cell is placed in a hypotonic solution, it will _________.
Your Score:
0%
0 / 0 correct