Vitamins Biochemistry: Organic compounds?
VITAMINS
Vitamins are organic compounds that are vital nutrients required in small amounts by the body for various metabolic functions, growth, and overall health.
With a few exceptions, the human body cannot synthesize vitamins on its own (or cannot synthesize them in sufficient quantities to meet physiological needs), and therefore they must be obtained through the diet.
- Non-caloric: Unlike carbohydrates, fats, and proteins, vitamins do not provide energy (calories) directly. Their role is to facilitate the processes that extract energy from macronutrients and to support other bodily functions.
- Micronutrients: They are classified as micronutrients because they are needed in much smaller quantities (milligrams or micrograms) compared to macronutrients.
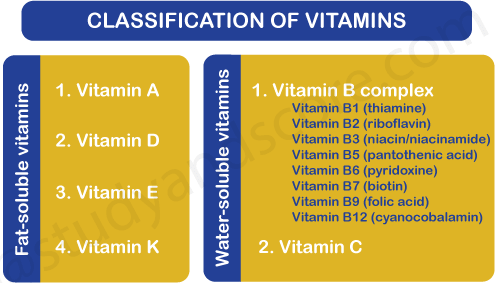
Classification of Vitamins
Vitamins are broadly categorized into two main groups based on their solubility:
A. Fat-Soluble Vitamins
Vitamins Included: Vitamin A, Vitamin D, Vitamin E, and Vitamin K (remembered by the mnemonic ADEK).
Key Characteristics:
- Absorption: Absorbed along with dietary fats, requiring bile salts and micelles.
- Transport: Incorporated into chylomicrons and transported through the lymphatic system before entering the bloodstream.
- Storage: The body has significant storage capacity, primarily in the liver and adipose tissues.
- Excretion: Not readily excreted; they tend to accumulate in the body.
- Toxicity: Higher potential for toxicity (hypervitaminosis) if consumed in excessive amounts, especially from supplements.
- Requirements: Generally required in smaller, less frequent doses.
B. Water-Soluble Vitamins
Vitamins Included: All the B-complex vitamins and Vitamin C.
B-complex vitamins: Thiamin (B1), Riboflavin (B2), Niacin (B3), Pantothenic Acid (B5), Pyridoxine (B6), Biotin (B7), Folate (B9), and Cobalamin (B12).
Key Characteristics:
- Absorption: Absorbed directly into the bloodstream from the small intestine (Vitamin B12 is a notable exception).
- Transport: Travel freely in the bloodstream.
- Storage: Minimal to no significant storage capacity (Vitamin B12 is a notable exception).
- Excretion: Excess amounts are readily excreted in the urine.
- Toxicity: Generally considered less toxic because excesses are flushed out, but very high doses can still be harmful.
- Requirements: Must be consumed more regularly (ideally daily) as they are not stored.
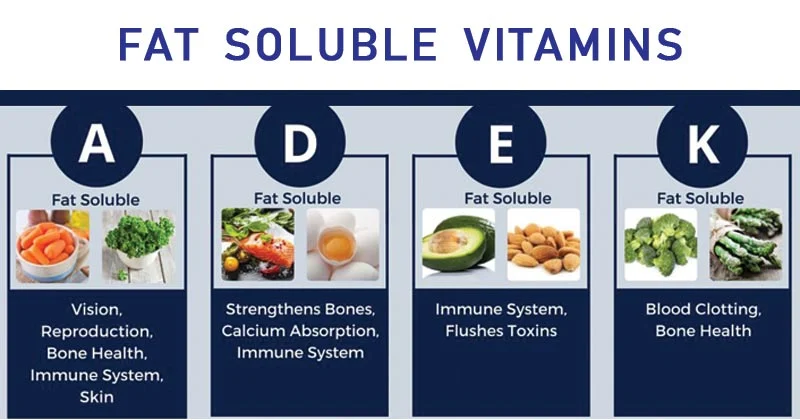
Fat-Soluble Vitamins (A, D, E, K)
1. Vitamin A
Forms:
- Retinoids: Preformed Vitamin A (retinol, retinal, retinoic acid) found in animal products. These are readily active in the body.
- Retinol: The primary alcohol form, circulated in the blood bound to retinol-binding protein (RBP). Once delivered to target cells, retinol can be reversibly oxidized to retinal by retinol dehydrogenases/reductases.
- Retinal: The aldehyde form, specifically 11-cis-retinal, is crucial for its role in vision. It is formed from all-trans-retinol in the retina.
- Retinoic acid: The carboxylic acid form, derived from the irreversible oxidation of retinal by retinal dehydrogenases. This form acts as a ligand for nuclear receptors.
- Beta-carotene, the most prominent provitamin A carotenoid, is symmetrically cleaved in the intestinal mucosa (and to a lesser extent in the liver) by the enzyme beta-carotene 15,15'-monooxygenase (BCMO1) to yield two molecules of retinal. Other carotenoids, like alpha-carotene and beta-cryptoxanthin, are cleaved asymmetrically to yield one molecule of retinal and one inactive product. This conversion process is regulated and not 100% efficient, which is why dietary recommendations use Retinol Activity Equivalents (RAE) to account for the differing bioavailabilities of preformed vitamin A versus provitamin A carotenoids.
Primary Functions:
- Vision: Crucial for light-dark adaptation and color vision (component of rhodopsin in the retina).
- In the rod cells of the retina, 11-cis-retinal binds covalently via a Schiff base to the opsin protein to form rhodopsin. When light (a photon) strikes rhodopsin, the 11-cis-retinal undergoes rapid photoisomerization to all-trans-retinal. This conformational change in the chromophore induces a conformational change in the opsin protein, activating a G-protein called transducin. This activation initiates a cGMP phosphodiesterase cascade, leading to the hydrolysis of cGMP, closure of cGMP-gated cation channels, hyperpolarization of the photoreceptor cell membrane, and ultimately the transmission of an electrical signal to the brain. For regeneration, all-trans-retinal is reduced to all-trans-retinol, transported out of the rod cell, isomerized to 11-cis-retinol in the retinal pigment epithelium, and then re-oxidized to 11-cis-retinal before returning to the rod cell.
- Cell Differentiation and Growth: Plays a role in maintaining epithelial tissues (skin, lining of respiratory, GI, and urinary tracts) and proper cell development.
- Retinoic acid functions as a powerful hormone. It diffuses into cells and binds to specific intracellular retinoic acid receptors (RARs) and retinoid X receptors (RXRs). These receptors are ligand-activated transcription factors. Upon ligand binding, the RAR/RXR heterodimer binds to specific DNA sequences called retinoic acid response elements (RAREs) in the promoter regions of target genes. This binding modulates gene expression (transcription), thereby controlling the proliferation, differentiation, and development of various cell types, particularly epithelial cells. For instance, it promotes the differentiation of immature epithelial cells into mature, specialized cells and suppresses keratinization.
- Immune Function: Supports the integrity of immune cells and their response.
- Through its gene regulatory actions via RARs and RXRs, retinoic acid influences the differentiation and function of various immune cells, including T cells (e.g., promoting Treg cell differentiation), B cells, and macrophages. It also modulates the expression of cytokines, chemokines, and adhesion molecules, impacting both innate and adaptive immune responses.
- Reproduction: Essential for normal reproductive function and embryonic development.
- Retinoic acid is critical for spermatogenesis in males and plays vital roles in ovarian function and placental development. In embryonic development, it precisely orchestrates pattern formation and organogenesis by regulating the expression of key developmental genes (e.g., Hox genes) along the anterior-posterior axis.
- Bone Health: Involved in bone remodeling.
- Retinoic acid influences the balance between bone formation (osteoblasts) and bone resorption (osteoclasts) by modulating the expression of various growth factors and cytokines involved in these processes.
Major Dietary Sources:
- Retinoids (Preformed Vitamin A): Liver, fish oil, dairy products (milk, cheese, butter), eggs.
- Carotenoids (Provitamin A): Orange and yellow fruits and vegetables (carrots, sweet potatoes, pumpkin, mango), dark leafy green vegetables (spinach, kale).
Consequences of Deficiency:
- Night blindness (Nyctalopia): The earliest and most common symptom, difficulty seeing in low light.
- Insufficient retinol supply leads to a lack of 11-cis-retinal, impairing the regeneration of rhodopsin. This reduces the sensitivity of rod photoreceptor cells, making it difficult to see in dim light.
- Xerophthalmia: A progressive drying of the conjunctiva and cornea of the eye, which can lead to blindness if untreated.
- Without adequate retinoic acid, the normal differentiation program of conjunctival goblet cells is disrupted, leading to a loss of mucus-secreting cells and their replacement by keratinizing squamous epithelium. This results in ocular dryness, keratinization, and ultimately corneal damage and opacification.
- Impaired Immune Function: Increased susceptibility to infections.
- The disruption of retinoic acid-dependent gene expression in immune cells compromises their development, proliferation, and ability to mount an effective immune response against pathogens. It also weakens the integrity of epithelial barriers.
- Follicular Hyperkeratosis: Rough, bumpy skin due to keratin accumulation.
- Similar to xerophthalmia, retinoic acid deficiency leads to abnormal differentiation of epidermal cells, promoting keratin synthesis and accumulation in hair follicles, resulting in thickened, bumpy skin.
- Stunted Growth: In children.
- Retinoic acid's role in cell proliferation and differentiation, and its interaction with growth factors, means its deficiency can impair normal growth and development.
Potential Risks and Symptoms of Toxicity (Hypervitaminosis A):
- Acute Toxicity: Nausea, vomiting, headache, blurred vision, muscle incoordination. Can occur from consuming very large single doses (e.g., polar bear liver).
- Extremely high doses can overwhelm transport and storage mechanisms, leading to the circulation of free, unbound retinol. Free retinol is amphipathic and can insert into cell membranes, increasing their fluidity and permeability, leading to cellular damage and lysis, especially in the liver and brain.
- Chronic Toxicity: Dry, itchy skin; hair loss; bone and joint pain; liver damage; birth defects (teratogenic); increased intracranial pressure.
- Sustained high levels of retinoic acid lead to aberrant gene expression. Teratogenicity is due to the exquisite sensitivity of embryonic development to the precise gradients of retinoic acid; excess disrupts these critical signals.
- Carotenemia: Excessive intake of carotenoids can lead to a harmless yellowish-orange discoloration of the skin. This is not true Vitamin A toxicity.
- The conversion of beta-carotene to retinal is regulated and decreases at high intake, preventing vitamin A toxicity. The yellowish hue results from the accumulation of these pigments in the skin.
2. Vitamin D
Forms:
- Vitamin
D₂(Ergocalciferol): Found in plant foods (e.g., mushrooms) and fortified foods. - Vitamin
D₃(Cholecalciferol): Synthesized in the skin upon exposure to ultraviolet B (UVB) sunlight, and found in animal foods (e.g., fatty fish). Both are converted to the active form, calcitriol.
Activation Pathway:
- Synthesis in Skin (
D₃): In epidermal keratinocytes, 7-dehydrocholesterol absorbs UVB radiation (λ 290-315 nm), forming pre-vitaminD₃, which then isomerizes to cholecalciferol (D₃). - Liver Hydroxylation: Both dietary
D₂andD₃are transported to the liver and hydroxylated to form 25-hydroxyvitamin D [25(OH)D] (calcidiol). This is the main circulating form. - Kidney Hydroxylation (Activation): 25(OH)D travels to the kidneys and undergoes a second hydroxylation to form 1,25-dihydroxyvitamin D [1,25(OH)₂D] (calcitriol), the biologically active hormone.
- Regulation of Activation: The final step is stimulated by parathyroid hormone (PTH) and low phosphate, and inhibited by high calcitriol (negative feedback).
Primary Functions:
- Calcium and Phosphorus Homeostasis: Primary role is to regulate blood levels of calcium and phosphorus.
- Calcitriol functions as a steroid hormone, binding to the Vitamin D Receptor (VDR). The VDR complex binds to Vitamin D Response Elements (VDREs) in DNA to regulate gene transcription, enhancing calcium absorption in the intestine, reabsorption in the kidneys, and mobilization from bone.
- Bone Mineralization: Essential for the proper formation and maintenance of bones by ensuring the availability of calcium and phosphate for hydroxyapatite crystals.
- Immune Function: VDRs are present on immune cells, and calcitriol influences their differentiation and cytokine production.
- Cell Growth and Differentiation: Influences cell cycle progression and apoptosis in a range of tissues.
Major Dietary Sources:
Fatty fish (salmon, mackerel), fortified foods (milk, yogurt, cereals), and sunlight exposure.
Consequences of Deficiency:
- Rickets: In children, characterized by impaired bone mineralization, leading to soft, weak bones, bowed legs, and skeletal deformities.
- Inadequate calcitriol leads to hypocalcemia. The resulting secondary hyperparathyroidism increases bone resorption, but the newly formed bone matrix (osteoid) cannot be properly mineralized, remaining soft.
- Osteomalacia: In adults, characterized by softening of the bones, leading to bone pain and increased fracture risk.
- Osteoporosis: Chronic insufficiency impairs calcium absorption and can lead to increased PTH levels, promoting bone loss.
Potential Risks and Symptoms of Toxicity (Hypervitaminosis D):
- Causes: Almost exclusively from over-supplementation.
- Symptoms: Hypercalcemia (high blood calcium), leading to nausea, vomiting, weakness, and frequent urination.
- Severe Toxicity: Can cause calcium deposits in soft tissues (kidneys, heart, blood vessels), leading to organ damage like nephrocalcinosis.
3. Vitamin E
Forms:
A group of eight compounds, including four tocopherols and four tocotrienols. Alpha-tocopherol is the most biologically active form in humans.
Primary Functions:
- Antioxidant: The primary function. It protects cell membranes and lipoproteins from oxidative damage.
- Vitamin E is a lipid-soluble, chain-breaking antioxidant embedded in membranes. It donates a hydrogen atom to neutralize highly reactive lipid peroxyl radicals (LOO•), preventing the propagation of lipid peroxidation. The resulting Vitamin E radical can be regenerated by Vitamin C.
- Immune Function & Anti-inflammatory: Supports immune cell health and may modulate inflammatory pathways.
Major Dietary Sources:
Vegetable oils, nuts and seeds (almonds, sunflower seeds), and leafy green vegetables.
Consequences of Deficiency:
- Rare: Clinical deficiency is rare in healthy individuals.
- Risk groups: Premature infants and individuals with fat malabsorption disorders.
- Symptoms: Neurological symptoms (muscle weakness, impaired coordination) and hemolytic anemia (rupture of red blood cells).
- Tissues with high PUFA content (e.g., neuronal and red blood cell membranes) are particularly vulnerable to oxidative stress without sufficient Vitamin E.
Potential Risks and Symptoms of Toxicity (Hypervitaminosis E):
- Primary Risk: High doses can interfere with blood clotting and potentiate the effects of anticoagulant medications (like warfarin), increasing the risk of hemorrhage.
- High concentrations of alpha-tocopherol can interfere with Vitamin K absorption and inhibit the activity of the Vitamin K-dependent enzyme gamma-glutamyl carboxylase.
4. Vitamin K
Forms:
- Vitamin
K₁(Phylloquinone): Found in plant foods. - Vitamin
K₂(Menaquinone): Produced by gut bacteria and found in some animal products.
Primary Functions:
- Blood Clotting (Coagulation): Essential for the synthesis of several blood clotting factors.
- Vitamin K is an essential cofactor for the enzyme gamma-glutamyl carboxylase. This enzyme modifies glutamate (Glu) residues on clotting factors (Prothrombin, Factors VII, IX, X) into gamma-carboxyglutamate (Gla). The Gla residues are critical for binding calcium ions (Ca²⁺), which is necessary for the clotting factors to anchor to phospholipid surfaces and participate in the coagulation cascade. The cycle of Vitamin K regeneration is the target of the anticoagulant drug warfarin.
- Bone Metabolism: Involved in the carboxylation of osteocalcin, a protein crucial for bone mineralization.
Major Dietary Sources:
Leafy green vegetables (kale, spinach, broccoli), soybean and canola oils. Gut bacteria also contribute significantly.
Consequences of Deficiency:
- Hemorrhage/Bleeding: The primary symptom due to impaired blood clotting.
- Without sufficient Vitamin K, clotting factors are under-carboxylated (PIVKAs). These proteins cannot bind calcium effectively and are biologically inactive, severely impairing the coagulation cascade.
- Newborns: Particularly susceptible (Hemorrhagic Disease of the Newborn) and are routinely given a Vitamin K injection at birth.
Potential Risks and Symptoms of Toxicity (Hypervitaminosis K):
- Very Rare: Toxicity from natural forms is extremely rare.
- Synthetic K (Menadione/
K₃): High doses of this synthetic form were associated with hemolytic anemia and liver damage. - Clinical Relevance: Excessive intake can antagonize the effects of anticoagulant medications (warfarin).
- Warfarin inhibits the enzyme (VKORC1) that recycles Vitamin K. A high intake of Vitamin K can overcome this inhibition, reducing the drug's effectiveness.
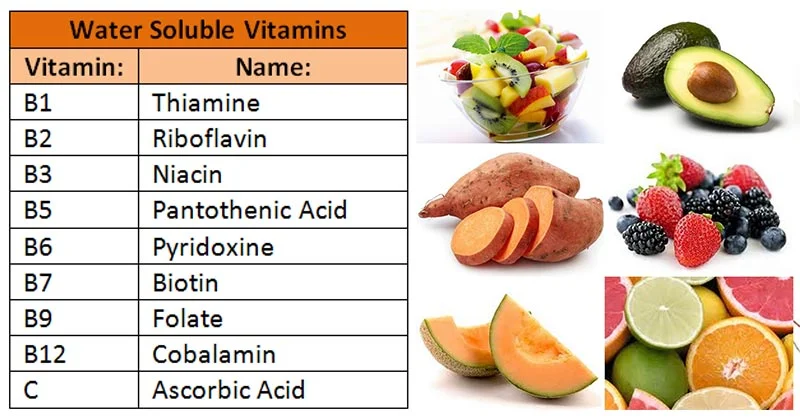
Water-Soluble Vitamins (B-Complex and C)
General Characteristics Reminder:
- Absorbed directly into the bloodstream: Unlike fat-soluble vitamins, water-soluble vitamins do not require bile salts for absorption and are typically absorbed directly into the portal circulation from the small intestine, bypassing the lymphatic system.
- Minimal body storage (except B12): Due to their water solubility, these vitamins are not stored extensively in adipose tissue or the liver (with the significant exception of Vitamin B₁₂). This lack of substantial storage means they need to be consumed regularly.
- Excess excreted in urine: When intake exceeds the body's immediate needs, the surplus water-soluble vitamins are readily filtered by the kidneys and excreted in the urine. This is a primary reason for their generally lower toxicity.
- Generally lower toxicity risk, but high doses of some can still be harmful: While less toxic than fat-soluble vitamins, certain water-soluble vitamins, particularly Vitamin B₆ and Niacin, can cause adverse effects at very high supplemental doses.
- Must be consumed regularly: Because they are minimally stored and readily excreted, a consistent dietary intake of water-soluble vitamins is essential to maintain adequate tissue concentrations and support metabolic functions.
1. Vitamin C (Ascorbic Acid)
Primary Functions:
- Collagen Synthesis: Crucial for wound healing and tissue integrity. Biochemical Detail: Acts as a cofactor for prolyl and lysyl hydroxylase, enzymes essential for the hydroxylation of proline and lysine residues in procollagen, which is vital for forming stable collagen triple-helices.
- Antioxidant: A powerful water-soluble antioxidant. Biochemical Detail: Directly neutralizes reactive oxygen species (ROS) like superoxide (
O₂∙⁻) and hydroxyl radicals (OH∙) by donating electrons. It also regenerates other antioxidants like Vitamin E. - Iron Absorption: Enhances the absorption of non-heme iron. Biochemical Detail: Reduces dietary ferric iron (
Fe³⁺) to the more absorbable ferrous iron (Fe²⁺) and forms a soluble chelate, preventing the formation of insoluble iron compounds. - Immune Function: Supports various aspects of the immune system by protecting immune cells from oxidative damage and enhancing their function.
- Neurotransmitter Synthesis: Biochemical Detail: It is a cofactor for dopamine β-hydroxylase, which converts dopamine to norepinephrine.
Major Dietary Sources:
Citrus fruits, strawberries, kiwis, bell peppers, broccoli, tomatoes.
Consequences of Deficiency (Scurvy):
Biochemical Basis: Impaired collagen synthesis. Symptoms include swollen, bleeding gums, impaired wound healing, petechiae (capillary fragility), joint pain, and anemia.
Potential Risks of Toxicity:
Relatively low toxicity. High doses (>2g/day) can cause GI distress (nausea, diarrhea). In susceptible individuals, may increase the risk of oxalate kidney stones or exacerbate iron overload in those with hemochromatosis.
2. B-Complex Vitamins
The B vitamins often work together and are frequently found in the same foods. Their primary role is as coenzymes in metabolic pathways, particularly those involved in energy production.
a) Thiamin (Vitamin B₁)
Primary Functions:
- Coenzyme: Its active form, thiamin pyrophosphate (TPP), is a crucial coenzyme in carbohydrate and amino acid metabolism. Biochemical Detail: TPP is required for key enzymes like the pyruvate dehydrogenase complex (linking glycolysis to the TCA cycle), α-ketoglutarate dehydrogenase (in the TCA cycle), and transketolase (in the pentose phosphate pathway).
- Nerve Function: Essential for nerve cell function, involved in neurotransmitter synthesis (acetylcholine) and maintaining the myelin sheath.
Major Dietary Sources:
Whole grains, enriched cereals, pork, legumes, nuts.
Consequences of Deficiency:
Beriberi: Biochemical Basis: Impaired TPP-dependent enzymes lead to reduced ATP production, affecting high-energy tissues.
- Wet Beriberi: Affects the cardiovascular system (edema, heart failure).
- Dry Beriberi: Affects the nervous system (muscle wasting, paralysis).
Wernicke-Korsakoff Syndrome: Seen in alcoholics due to poor diet and impaired absorption, causing severe neurological symptoms.
Toxicity:
No known toxicity from oral intake.
b) Riboflavin (Vitamin B₂)
Primary Functions:
- Coenzyme: Component of FAD (flavin adenine dinucleotide) and FMN (flavin mononucleotide). Biochemical Detail: These act as electron carriers in oxidation-reduction reactions. They are essential for the electron transport chain (Complex I and II), fatty acid β-oxidation, and the activation of other vitamins like B₆.
Major Dietary Sources:
Milk and dairy products, enriched grains, leafy green vegetables, liver.
Consequences of Deficiency (Ariboflavinosis):
Symptoms include cheilosis (cracks at mouth corners), glossitis (magenta tongue), and seborrheic dermatitis. Biochemical Basis: Impaired cellular energy metabolism in rapidly dividing cells.
Toxicity:
No known toxicity from oral intake.
c) Niacin (Vitamin B₃)
Primary Functions:
- Coenzyme: Component of
NAD⁺(nicotinamide adenine dinucleotide) andNADP⁺(nicotinamide adenine dinucleotide phosphate). Biochemical Detail:NAD⁺is a key electron acceptor in catabolic pathways (glycolysis, TCA cycle), forming NADH for ATP production.NADP⁺is reduced to NADPH, which serves as a primary reducing agent in anabolic pathways (fatty acid synthesis, cholesterol synthesis).
Major Dietary Sources:
Meat, poultry, fish, enriched grains, peanuts. Can also be synthesized from tryptophan.
Consequences of Deficiency (Pellagra):
Characterized by the "4 D's": Dermatitis, Diarrhea, Dementia, and Death. Biochemical Basis: Widespread metabolic dysfunction due to lack of NAD⁺ and NADP⁺.
Potential Risks of Toxicity:
High doses of nicotinic acid can cause a "Niacin Flush" (due to prostaglandin release), GI distress, and in rare cases, liver damage. Used pharmacologically to lower LDL cholesterol.
d) Pantothenic Acid (Vitamin B₅)
Primary Functions:
- Coenzyme A (CoA) Component: Essential component of Coenzyme A. Biochemical Detail: CoA is a central molecule in metabolism, serving as an acyl group carrier. The thiol group (
-SH) of CoA forms high-energy thioester bonds (e.g., acetyl-CoA, succinyl-CoA), enabling the transfer of acyl groups in the TCA cycle, fatty acid synthesis/oxidation, and cholesterol synthesis.
Major Dietary Sources:
Widespread in almost all foods (from Greek "pantos," meaning "from everywhere"). Liver, eggs, broccoli, whole grains.
Consequences of Deficiency:
Extremely rare. Symptoms include fatigue and "burning feet" syndrome.
Toxicity:
No known toxicity from oral intake.
e) Pyridoxine (Vitamin B₆)
Primary Functions:
- Coenzyme: Active form is pyridoxal phosphate (PLP), involved in over 100 enzyme reactions, primarily in amino acid metabolism. Biochemical Detail: PLP is a coenzyme for transamination (synthesis/degradation of amino acids) and decarboxylation reactions (synthesis of neurotransmitters like serotonin, dopamine, and GABA).
- Heme Synthesis: PLP is a coenzyme for ALAS, the rate-limiting enzyme in heme biosynthesis.
- Glycogenolysis: PLP is a coenzyme for glycogen phosphorylase, which breaks down glycogen.
Major Dietary Sources:
Meat, fish, potatoes, bananas, whole grains.
Consequences of Deficiency:
Symptoms include seborrheic dermatitis, microcytic anemia (due to impaired heme synthesis), depression, confusion, and convulsions (due to impaired GABA synthesis).
Potential Risks of Toxicity:
High doses from supplements can cause irreversible sensory neuropathy (nerve damage).
f) Biotin (Vitamin B₇)
Primary Functions:
- Coenzyme: Acts as a coenzyme for carboxylase enzymes. Biochemical Detail: Biotin facilitates the transfer of carboxyl groups (
-COO⁻). It is essential for pyruvate carboxylase (in gluconeogenesis), acetyl-CoA carboxylase (in fatty acid synthesis), and propionyl-CoA carboxylase (in amino acid metabolism).
Major Dietary Sources:
Egg yolks, liver, nuts, soybeans. Also produced by gut bacteria.
Consequences of Deficiency:
Extremely rare. Can be induced by consuming large amounts of raw egg whites, which contain avidin, a protein that binds biotin. Symptoms include hair loss, skin rash, and neurological problems.
Toxicity:
No known toxicity from oral intake.
g) Folate (Vitamin B₉)
Primary Functions:
- DNA Synthesis and Repair: Crucial for cell division and growth. Biochemical Detail: The active form, tetrahydrofolate (FH₄), is a carrier of one-carbon units. It is essential for the synthesis of purines (adenosine, guanosine) and thymidylate, which are required for DNA replication.
- Amino Acid Metabolism: Involved in the conversion of homocysteine to methionine (requires B₁₂).
Major Dietary Sources:
Dark leafy green vegetables (spinach, asparagus), legumes, liver, and fortified grains (as folic acid).
Consequences of Deficiency:
Megaloblastic Anemia: Biochemical Basis: Impaired DNA synthesis prevents proper cell division in RBC precursors, leading to large, immature cells (megaloblasts) that are prematurely destroyed.
Neural Tube Defects (NTDs): Severe birth defects (e.g., spina bifida). Adequate intake before and during early pregnancy is critical for the proper closure of the neural tube.
Potential Risks of Toxicity:
High doses of folic acid can mask a Vitamin B₁₂ deficiency, allowing the irreversible neurological damage of B₁₂ deficiency to progress unnoticed.
h) Cobalamin (Vitamin B₁₂)
Primary Functions:
- Coenzyme: Essential for two major enzyme reactions. Biochemical Detail:
- Acts as a coenzyme for methionine synthase to convert homocysteine to methionine (linked to folate metabolism).
- Acts as a coenzyme for methylmalonyl-CoA mutase to convert methylmalonyl-CoA to succinyl-CoA (essential for metabolizing odd-chain fatty acids).
- Nervous System Function: Crucial for maintaining the myelin sheath. Biochemical Basis: Deficiency leads to the accumulation of methylmalonic acid (MMA), which disrupts lipid synthesis and leads to abnormal fatty acids being incorporated into myelin.
- Red Blood Cell Formation: Indirectly involved in DNA synthesis via its role in regenerating tetrahydrofolate (the "folate trap").
Major Dietary Sources:
Only found naturally in animal products: meat, poultry, fish, eggs, dairy.
Consequences of Deficiency:
Pernicious Anemia: Megaloblastic anemia caused by a lack of intrinsic factor (a protein required for B₁₂ absorption), often due to an autoimmune condition.
Megaloblastic Anemia: Similar to folate deficiency.
Irreversible Neurological Damage: The most serious consequence, which can occur even without anemia. Symptoms include numbness, tingling, difficulty walking, and memory loss.
Toxicity:
No known toxicity from oral intake. The body stores several years' worth in the liver.
Misconceptions and Current Issues
This section addresses common misunderstandings about vitamin supplementation and delves into the ongoing debate surrounding optimal nutrient intake versus established recommendations. It’s crucial to understand these nuances for informed health decisions.
I. Addressing Misconceptions About Vitamin Supplementation
"More is Always Better":
- Misconception: Many believe that if a little of a vitamin is good, a lot must be even better, especially for health and performance. This often stems from a simplistic view of nutrient function, ignoring dose-response relationships and homeostatic regulation.
- Reality: This is often untrue and can be dangerous, particularly for fat-soluble vitamins (A, D, E, K) and some water-soluble vitamins (Niacin, B₆). Excessive intake can lead to toxicity (hypervitaminosis), causing adverse health effects, sometimes irreversible. Even for water-soluble vitamins, extremely high doses can cause gastrointestinal upset or other specific issues. The body has optimal levels; exceeding them provides no additional benefit and often carries risks.
- Biochemical and Physiological Detail: The body has intricate homeostatic mechanisms to maintain nutrient levels within a narrow physiological range.
- Fat-Soluble Vitamins: Because they are stored in adipose tissue and the liver, excess intake can accumulate to toxic levels.
- Hypervitaminosis A: Excessive preformed Vitamin A can cause acute (nausea, headache) or chronic (bone pain, liver damage, birth defects) toxicity.
- Hypervitaminosis D: Leads to hypercalcemia (excessive calcium in the blood), which can cause calcification of soft tissues (kidneys, blood vessels) and kidney damage.
- Water-Soluble Vitamins: While generally excreted, some have toxic thresholds.
- Niacin (Nicotinic Acid): High doses cause vasodilation (niacin flush) and can lead to liver damage and increased insulin resistance.
- Vitamin B₆ (Pyridoxine): Very high doses can cause sensory neuropathy due to direct neurotoxicity, leading to demyelination and axonal degeneration.
- Vitamin C: Extremely high doses (>2g/day) can cause osmotic diarrhea and may increase the risk of oxalate kidney stones in predisposed individuals.
- Beyond Optimal: Once the coenzyme sites are saturated or physiological functions are maximally supported, further intake provides no additional benefit. Instead, the body must metabolize and excrete the excess.
- Fat-Soluble Vitamins: Because they are stored in adipose tissue and the liver, excess intake can accumulate to toxic levels.
"Supplements Can Replace a Healthy Diet":
- Misconception: Some people rely on supplements as a "nutritional safety net" to compensate for a poor diet, believing they can get all necessary nutrients from pills.
- Reality: Food provides a complex matrix of vitamins, minerals, fiber, antioxidants, and phytochemicals that work synergistically. Supplements typically isolate a few nutrients. A varied diet of whole foods offers a broader spectrum of beneficial compounds and better absorption. Supplements are meant to supplement the diet, not replace it.
- Biochemical and Physiological Detail:
- Food Synergy: The health benefits of whole foods often arise from the synergistic interactions between various nutrients and non-nutrient bioactive compounds (e.g., flavonoids, carotenoids).
- Fiber: Whole foods provide dietary fiber, essential for gut health and modulating nutrient absorption, which is absent in most vitamin supplements.
- Absorption Differences: The food matrix can influence absorption patterns, often more favorably than isolated supplements.
"Natural Supplements Are Always Safe":
- Misconception: The term "natural" often implies safety or superiority, leading consumers to believe that products derived from natural sources are inherently benign.
- Reality: "Natural" doesn't automatically mean safe. Many natural substances can be toxic in high doses. Furthermore, the supplement industry is less regulated than pharmaceuticals, so product quality, purity, and content can vary greatly.
- Regulatory Aspects: Dietary supplements do not undergo the same rigorous pre-market testing for safety and efficacy as pharmaceuticals. This can lead to issues with contamination, inaccurate dosing, lack of efficacy, and negative interactions with medications.
"Supplements Give You Energy":
- Misconception: Many B-vitamin supplements are marketed as "energy boosters." This is often a marketing ploy that capitalizes on a partial truth.
- Reality: While B vitamins are crucial for energy metabolism (converting food into energy), they do not directly provide energy themselves (no calories). If you are deficient, supplementing can restore normal energy levels. However, if you are not deficient, taking more B vitamins will generally not provide a noticeable "energy boost."
- Biochemical Detail: B vitamins are coenzymes; they facilitate enzymatic reactions that release energy from macronutrients. In a non-deficient person, the coenzyme sites are already saturated, and adding more simply results in excretion, not enhanced energy production. Any perceived "energy boost" is often a placebo effect or due to other stimulant ingredients (e.g., caffeine).
"Supplements Are Always Effective for Preventing Disease":
- Misconception: Many assume taking specific vitamin supplements will prevent chronic diseases like heart disease or cancer.
- Reality: For the general healthy population, large-scale randomized controlled trials have often failed to show significant benefits of routine supplementation for preventing chronic diseases. In some cases (e.g., high-dose beta-carotene in smokers), supplementation has even shown adverse effects.
- Scientific Evidence:
- Large studies (ATBC, CARET) found that high-dose β-carotene supplementation in smokers increased the risk of lung cancer, possibly by acting as a pro-oxidant.
- Major trials on Vitamin E have generally found no benefit, and sometimes increased risk, for preventing cardiovascular disease or cancer.
- Numerous studies on multivitamins have concluded that they do not reduce the risk of major chronic diseases in generally healthy adults.
- Context Matters: Benefits of supplementation are most clear in specific contexts like deficiency correction (B₁₂ for pernicious anemia), for at-risk populations (folic acid for women of childbearing age), or for specific medical conditions.
II. Current Issues: Optimal Intake vs. Recommended Dietary Allowances (RDAs)
This distinction highlights a fundamental tension in nutritional science and public health guidance.
Recommended Dietary Allowances (RDAs) / Dietary Reference Intakes (DRIs):
- Purpose: These are science-based nutrient intake values established by health authorities.
- Goal: To define daily intake levels sufficient to meet the needs of nearly all (97-98%) healthy individuals. The primary goal is to prevent nutrient deficiencies and maintain basic physiological function.
- Focus: They represent minimums to avoid overt deficiency diseases (e.g., scurvy, pellagra). They are not necessarily designed to promote optimal health.
- Biochemical Basis: RDAs are typically set two standard deviations above the Estimated Average Requirement (EAR), aiming to cover the vast majority of the healthy population's needs for preventing deficiency.
Optimal Intake:
- Concept: This refers to the level of nutrient intake believed to provide maximum health benefits, enhance physiological function, and reduce the risk of chronic diseases, which may be higher than the RDA.
- Challenges: Defining "optimal intake" is complex and debated. It can vary significantly based on individual genetics, lifestyle, and health status.
- Individual Variability: Genetic polymorphisms (e.g., MTHFR gene and folate), lifestyle factors (smoking, stress), and chronic diseases can alter nutrient demands.
The Debate and Practical Implications:
- RDAs as a Baseline: RDAs remain the most widely accepted and practical guidelines for the general population.
- Supplementation Dilemma: The concept of "optimal intake" often fuels the supplement industry. While certain groups do have higher needs, routine high-dose supplementation for everyone is not universally supported by evidence.
- Risk vs. Benefit: For some nutrients, higher "optimal" intakes might bring higher risks of toxicity. The benefit-risk ratio needs careful consideration.
- Personalized Nutrition: There's a growing recognition that nutrient needs can be highly individualized. Future approaches may involve more personalized recommendations based on genomics (nutrigenomics), biomarkers, and lifestyle factors.
Summary of Key Takeaways for Vitamins:
- Essential, Non-Caloric: Vitamins are vital micronutrients that don't provide energy but enable its use by acting as coenzymes or regulatory molecules.
- Two Classes:
- Fat-soluble (A, D, E, K): Stored in the body, require dietary fat for absorption, higher toxicity risk.
- Water-soluble (B-complex, C): Minimal storage (except B₁₂), readily excreted, require regular intake, generally lower toxicity risk.
- Specific Roles: Each vitamin has unique and critical biochemical functions.
- Diet First: A balanced, varied diet of whole foods is the best source of vitamins.
- Bioavailability Matters: The amount of a vitamin consumed isn't always the amount the body utilizes.
- Prudent Supplementation: Supplements are beneficial for correcting deficiencies or for specific at-risk groups but cannot fully replicate the benefits of a healthy diet. "More is not always better."
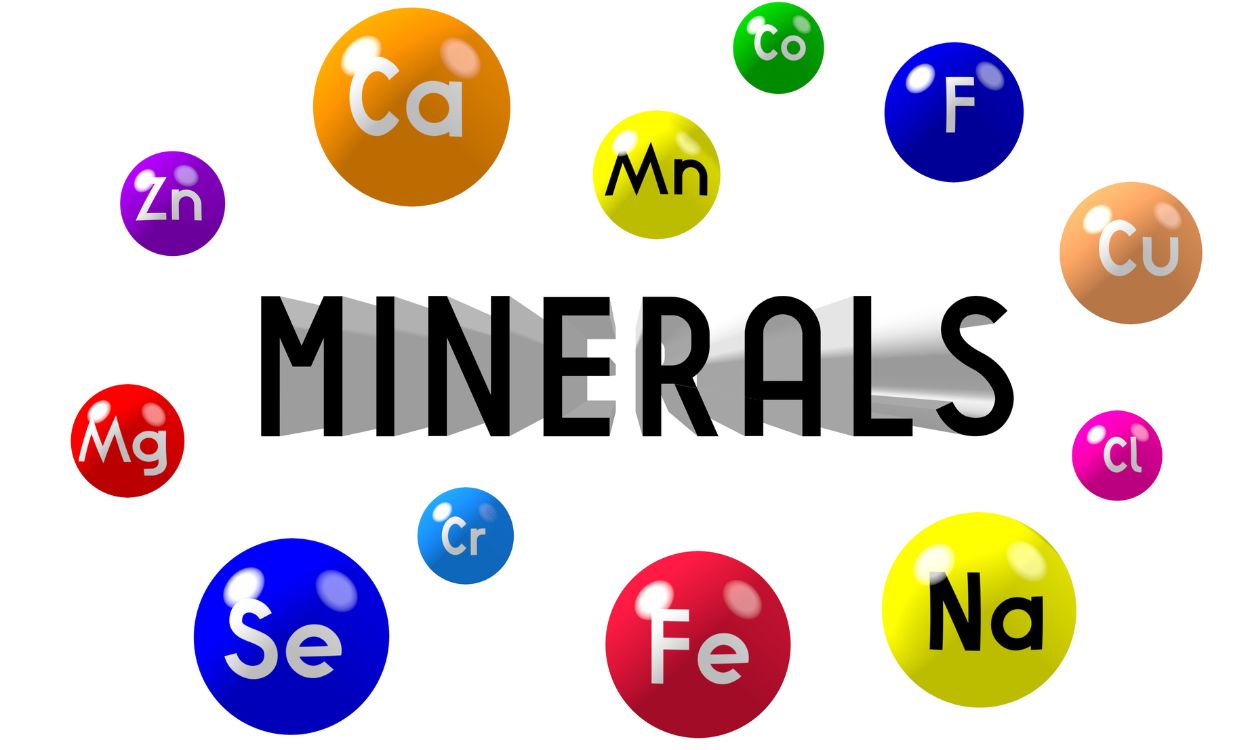
Minerals
Minerals are inorganic elements that originate in the earth and cannot be made by living organisms. Plants absorb minerals from the soil, and we obtain them by eating plants or animals that have eaten plants. 22 minerals are needed by the body. They are for maintaining bodily functions and are categorized into two groups based on the amounts needed by the body: macrominerals (or major minerals) and trace minerals (or microminerals).
I. Macrominerals (Major Minerals)
These are required in larger amounts ( >100 mg/day).
Calcium (Ca)
- Biological Roles:
- Bone and Teeth Health: The most abundant mineral in the body, primarily stored in bones and teeth, providing structural support.
- Muscle Function: Essential for muscle contraction and relaxation.
- Nerve Transmission: Plays a vital role in transmitting nerve impulses.
- Blood Clotting: A cofactor in several steps of the clotting cascade.
- Hormone Secretion: Involved in the release of various hormones.
- Dietary Sources: Dairy products (milk, yogurt, cheese), leafy green vegetables (kale, broccoli), fortified foods (cereals, orange juice), fish with edible bones (sardines, salmon).
- Examples: Yogurt (plain, low-fat): 415 mg/cup; Milk (skim/1-2%): ~300 mg/cup; Fortified orange juice: 300 mg/8 oz; Salmon (canned): 165 mg/3 oz; Broccoli (cooked): 68 mg/1/2 cup.
- Daily Requirements:
- Males 19-50 years old: 1,000 mg / day
- Females 19-50 years old: 1,000 mg / day
- Deficiency Symptoms: Osteoporosis (weak, brittle bones), muscle cramps, rickets (in children), impaired nerve function.
- Excess: Excessive intake can contribute to kidney stones.
Phosphorus (P)
- Biological Roles:
- Bone and Teeth Formation: Second most abundant mineral, also crucial for bones and teeth, often found as calcium phosphate.
- Energy Metabolism (ATP): A key component of ATP (adenosine triphosphate), the primary energy currency of the cell.
- Nucleic Acids: Forms the backbone of DNA and RNA.
- Cell Membranes: A vital part of phospholipids, which make up cell membranes.
- pH Balance: Helps maintain acid-base balance (as phosphate buffers).
- Dietary Sources: Meat, poultry, fish, eggs, dairy products, nuts, legumes, whole grains.
- Deficiency Symptoms: Rare, but can include bone pain, muscle weakness, confusion, and impaired immunity.
Potassium (K)
- Biological Roles:
- Fluid Balance: Works with sodium to maintain proper fluid balance inside and outside cells.
- Nerve Impulse Transmission: Critical for generating nerve impulses.
- Muscle Contraction: Essential for normal muscle function, including heart muscle.
- Blood Pressure Regulation: Helps counteract the effects of sodium, contributing to lower blood pressure.
- Dietary Sources: Fruits (bananas, oranges, avocados), vegetables (spinach, potatoes, sweet potatoes), legumes, nuts, milk, fish.
- Deficiency Symptoms (Hypokalemia): Muscle weakness, cramps, irregular heartbeat, fatigue.
Sodium (Na)
- Biological Roles:
- Fluid Balance: Major electrolyte involved in maintaining fluid balance, primarily outside cells.
- Nerve Impulse Transmission: Essential for nerve signaling.
- Muscle Contraction: Involved in muscle contraction.
- Nutrient Absorption: Aids in the absorption of certain nutrients (e.g., glucose, amino acids).
- Deficiency Symptoms (Hyponatremia): Nausea, vomiting, headache, confusion, muscle cramps, fatigue, seizures (severe).
- Daily Requirements:
- The human body requires about 500 mg of sodium per day.
- Recommended to stay in a range of 1,500 to 2,400 mg / day. (Average American ingests 2,300-6,900 mg/day).
- Dietary Sources: Processed foods (canned goods, frozen meals), table salt, cured meats, dairy products, condiments.
- Hidden Sodium on Food Labels: Monosodium glutamate (MSG), Baking soda, Baking powder, Disodium phosphate, Sodium alginate, Sodium nitrate or nitrite.
- Health Considerations:
- Deficiency (Hyponatremia): Rare in healthy individuals, usually due to excessive fluid loss.
- Excess: Too much sodium causes high blood pressure (hypertension) and may lead to fluid retention.
- Reducing Sodium in Diet: Eat more fresh foods, eat less processed foods, look for low-sodium products, limit added salt, and experiment with other seasonings.
Magnesium (Mg)
- Biological Roles:
- Enzyme Cofactor: Involved in over 300 biochemical reactions, including energy production, protein synthesis, and DNA synthesis.
- Muscle and Nerve Function: Critical for proper muscle and nerve function.
- Blood Glucose Control: Involved in blood sugar regulation.
- Blood Pressure Regulation: Contributes to maintaining healthy blood pressure.
- Bone Health: A component of bone structure.
- Dietary Sources: Leafy green vegetables (spinach, kale), nuts (almonds, cashews), seeds (pumpkin, chia), legumes, whole grains, dark chocolate, avocados.
- Deficiency Symptoms: Muscle cramps, fatigue, weakness, irregular heartbeat, nausea, loss of appetite.
Chloride (Cl)
- Biological Roles:
- Fluid Balance: Works with sodium to maintain fluid and electrolyte balance.
- Gastric Acid: A component of hydrochloric acid (HCl) in the stomach, essential for digestion.
- pH Balance: Plays a role in maintaining acid-base balance.
- Dietary Sources: Table salt (sodium chloride), processed foods, seaweed, olives.
- Deficiency Symptoms: Rare, can lead to metabolic alkalosis.
Sulfur (S)
- Biological Roles:
- Protein Structure: A component of amino acids (methionine, cysteine), forming disulfide bonds crucial for protein folding.
- Vitamin Component: Found in thiamin and biotin.
- Detoxification: Involved in detoxification pathways in the liver.
- Dietary Sources: Protein-rich foods (meat, poultry, fish, eggs, dairy), legumes, alliums (garlic, onions).
- Deficiency Symptoms: Extremely rare with adequate protein intake.
II. Trace Minerals (Microminerals)
These are required in smaller amounts (<100 mg/day), but are just as vital.
Iron (Fe)
- Biological Roles:
- Oxygen Transport: Key component of hemoglobin (in red blood cells) and myoglobin (in muscle cells).
- Energy Production: Involved in enzymes critical for energy metabolism.
- Immune Function: Supports a healthy immune system.
- Dietary Sources:
- Heme Iron: Found in animal products; highly absorbable (Red meats, liver, poultry).
- Non-Heme Iron: Found in plant products; less absorbable, but absorption is enhanced by Vitamin C (Beans, lentils, spinach, fortified cereals).
- Deficiency Symptoms (Anemia): Fatigue, weakness, shortness of breath, pale skin, impaired cognitive function.
Zinc (Zn)
- Biological Roles:
- Enzyme Cofactor: Involved in over 300 enzymes (metabolism, DNA synthesis, cell division).
- Immune Function: Crucial for immune cell development and function.
- Wound Healing: Essential for tissue repair.
- Taste and Smell: Important for these senses.
- Dietary Sources: Oysters, red meat, poultry, beans, nuts, whole grains.
- Deficiency Symptoms: Impaired immune function, poor wound healing, hair loss, loss of appetite, delayed growth.
Copper (Cu)
- Biological Roles:
- Iron Metabolism: Essential for iron absorption and utilization.
- Energy Production: Component of enzymes in energy metabolism.
- Connective Tissue Formation: Crucial for the formation of collagen and elastin.
- Antioxidant Defense: Part of superoxide dismutase.
- Dietary Sources: Organ meats, shellfish, nuts, seeds, whole grains, chocolate.
- Deficiency Symptoms: Rare, but can include anemia, bone abnormalities, impaired immune function.
Manganese (Mn)
- Biological Roles: Cofactor for enzymes in bone formation, metabolism, and antioxidant defense (superoxide dismutase).
- Dietary Sources: Whole grains, nuts, legumes, leafy green vegetables, tea.
- Deficiency Symptoms: Rare, but can include impaired growth and skeletal abnormalities.
Iodine (I)
- Biological Roles: Essential component of thyroid hormones (T3 and T4), which regulate metabolism, growth, and development.
- Dietary Sources: Iodized salt, seafood (fish, seaweed), dairy products.
- Deficiency Symptoms: Goiter (enlarged thyroid gland), hypothyroidism, cretinism (severe developmental delay in infants).
Selenium (Se)
- Biological Roles: Key component of selenoproteins with antioxidant roles (e.g., glutathione peroxidase), involved in thyroid function and immunity.
- Dietary Sources: Brazil nuts, seafood, organ meats, meat, grains.
- Deficiency Symptoms: Rare, but can lead to Keshan disease (a form of cardiomyopathy).
Chromium (Cr)
- Biological Roles: Enhances the action of insulin, helping regulate blood glucose levels.
- Dietary Sources: Whole grains, lean meats, brewer's yeast, some fruits and vegetables.
- Deficiency Symptoms: Impaired glucose tolerance, elevated blood sugar.
Fluoride (F)
- Biological Roles: Strengthens tooth enamel and contributes to bone density.
- Dietary Sources: Fluoridated water, tea, seafood.
- Deficiency Symptoms: Increased risk of dental caries (cavities).
Molybdenum (Mo)
- Biological Roles: Cofactor for enzymes involved in metabolism of sulfur-containing amino acids, DNA, and uric acid.
- Dietary Sources: Legumes, grains, nuts, leafy green vegetables.
- Health Considerations: Deficiency is extremely rare in humans.
Arsenic (As)
- Biological Roles (Trace): Ultra-trace amounts may play a role in metabolism in some animal species, but its essentiality in humans is not established.
- Health Considerations: Known carcinogen and toxicant at higher levels.
Nickel (Ni)
- Biological Roles (Trace): Considered essential in some animal species; precise role in humans is still under investigation.
- Health Considerations: Deficiency is not well-defined in humans. Can be an allergen.
Silicon (Si)
- Biological Roles (Trace): Appears to be involved in bone formation and connective tissue health.
- Dietary Sources (Trace): Whole grains, root vegetables, beer, water.
Boron (B)
- Biological Roles (Trace): Thought to play a role in bone metabolism, brain function, and hormone regulation.
- Dietary Sources (Trace): Fruits, vegetables, nuts, legumes.
Cobalt (Co)
- Biological Roles (Trace): Essential as a central component of vitamin B12 (cobalamin).
- Dietary Sources: Meat, fish, dairy (indirectly, as B12 is found in animal products).
- Health Considerations: Deficiency is related to inadequate vitamin B12 intake, leading to pernicious anemia.
Considerations:
- Bioavailability: Not all minerals in food are absorbed equally. Factors like other food components and digestive health can affect absorption.
- Interactions: Minerals can interact with each other. High intake of one can sometimes interfere with the absorption of another.
- Toxicity: While essential, minerals can be toxic if consumed in excessively high amounts, often from supplements.
- Balance: The key is a balanced intake from a varied diet to ensure adequate amounts of all essential minerals without excesses.