Muscle Tissue: The Body's Engine of Movement
Muscle Tissue
Muscle tissue is composed of highly specialized, contractile cells that generate force to produce movement. The cells within all three types of muscle tissue are specialized for contraction (shortening), a process enabled by the interaction of specialized protein fibers. This contraction enables the movement of the whole body and many internal organs, in addition to producing heat energy.
An important characteristic is that mature muscle cells have generally lost the ability to divide, so destroyed muscle cells often cannot be replaced.
General Characteristics
All muscle tissues share a set of key properties that allow them to function effectively.
Excitability (Responsiveness)
The ability to receive and respond to a stimulus (like a nerve impulse).
Contractility
The ability to shorten forcibly when stimulated.
Extensibility
The ability to be stretched or extended.
Elasticity
The ability to recoil and resume its resting length after stretching.
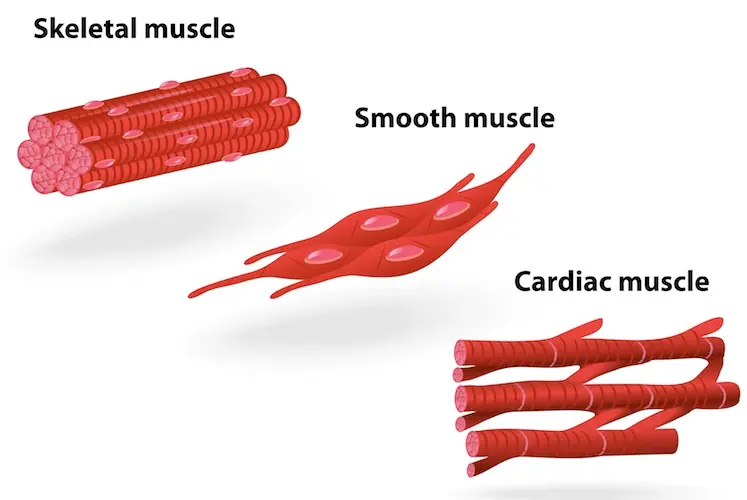
The Three Types of Muscle Tissue
Muscle tissue is classified into three types based on location, structure, and functional characteristics. While the cells in smooth and cardiac muscle are referred to as muscle cells, the long, cylindrical cells of skeletal muscle are often called muscle fibers.
1. Skeletal Muscle
(Striped appearance)
(Under conscious control)
(Long, cylindrical cells)
Location: Primarily attached to the skeleton, enabling body movement.
2. Cardiac Muscle
(Striped appearance)
(Not under conscious control)
(Connected by intercalated discs)
Location: Found exclusively in the wall of the heart.
3. Smooth Muscle
(Smooth appearance)
(Not under conscious control)
(Single central nucleus)
Location: Found in the walls of hollow organs like the stomach, bladder, and blood vessels.
Skeletal Muscle
Named for its location, skeletal muscle tissue is usually attached to bones and skin, enabling movement of the head, trunk, and limbs. Its contractions are voluntary (under conscious control).
Key Characteristics:
- Striated: Appears striped or banded due to the highly organized arrangement of contractile proteins (actin and myosin).
- Voluntary: Contraction is consciously controlled by the nervous system.
- Multi-nucleated Fibers: The cells (muscle fibers) are long, cylindrical, and contain multiple nuclei located at the periphery.
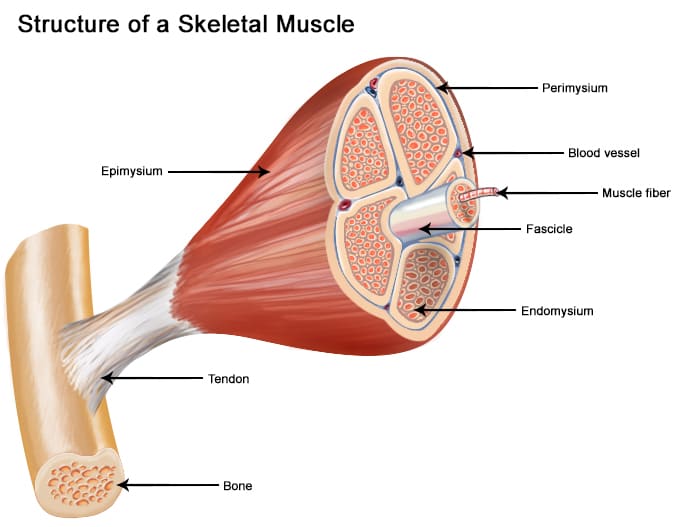
General Organization (Macroscopic to Microscopic)
A whole skeletal muscle is a complex organ containing muscle fibers, blood vessels, nerve fibers, and extensive connective tissue wrappings that hold everything together and transmit the force of contraction.
1. Entire Muscle
The whole organ, surrounded by a dense irregular CT layer called the Epimysium.
2. Muscle Fascicle
A bundle of muscle fibers, surrounded by a fibrous CT layer called the Perimysium.
3. Muscle Fiber (Cell)
A single muscle cell, surrounded by a delicate areolar CT layer called the Endomysium.
These three "mysiums" are continuous and converge to form tendons, which transmit the contractile force to the bones.

Microscopic Organization of a Muscle Fiber
A skeletal muscle fiber is a highly specialized, elongated cell optimized for rapid and powerful contraction.
Sarcolemma & Sarcoplasm
The Sarcolemma is the cell membrane, featuring deep invaginations called T-tubules. The Sarcoplasm is the cytoplasm, rich in glycogen (glycosomes) and oxygen-storing myoglobin.
Sarcoplasmic Reticulum (SR)
A specialized smooth ER that surrounds each myofibril. Its primary role is to store and release calcium ions (Ca²⁺), the critical trigger for muscle contraction.
Myofibrils and the Sarcomere
Myofibrils are the rod-like contractile elements that make up ~80% of the muscle fiber's volume. Each myofibril is a chain of repeating sarcomeres, the smallest functional unit of muscle contraction.
Sarcomere Banding Pattern (Striations)
- A-Band (Dark): Represents the full length of the thick (myosin) filaments.
- I-Band (Light): Contains only thin (actin) filaments.
- Z-Disc (Line): A protein sheet that anchors thin filaments and defines the boundaries of one sarcomere.
Myofilaments (Contractile Proteins)
- Thick Filaments (Myosin): Composed of myosin protein with globular heads that bind to actin and use ATP to generate force.
- Thin Filaments (Actin): Composed of actin protein, which has binding sites for myosin heads. Also contains two regulatory proteins:
- Tropomyosin: Blocks the myosin-binding sites on actin in a relaxed muscle.
- Troponin: Binds to Ca²⁺, which causes it to move tropomyosin, exposing the binding sites and allowing contraction to begin.
The Sliding Filament Model of Contraction
This is how muscles contract:
- A nerve impulse triggers the release of Ca²⁺ from the Sarcoplasmic Reticulum.
- Ca²⁺ binds to troponin, causing it to move tropomyosin away from actin's binding sites.
- Myosin heads bind to actin, forming a cross-bridge.
- The myosin heads pivot, pulling the thin filaments toward the center of the sarcomere (the "power stroke"). This uses ATP.
- The myosin head detaches, re-cocks, and is ready for another cycle as long as Ca²⁺ and ATP are present.
This sliding action shortens all the sarcomeres simultaneously, causing the entire muscle fiber to contract.
Satellite Cells
These are quiescent (inactive) stem cells located on the surface of mature muscle fibers. When a muscle fiber is injured, satellite cells become activated. They divide and differentiate into new muscle cells to repair the damaged tissue and also contribute to muscle growth (hypertrophy) in response to exercise.
Cardiac Muscle Tissue
The muscle tissue located in the walls of the heart is cardiac muscle tissue. It consists of branching cells that interconnect in a netlike arrangement. The rhythmic contractions of cardiac muscle are involuntary because they cannot be consciously controlled.
General Characteristics
- Location: Found exclusively in the myocardium, the middle and thickest layer of the heart wall.
- Function: Responsible for the forceful, rhythmic contractions that pump blood throughout the body.
- Control: Involuntary. It possesses its own intrinsic electrical conduction system (autorhythmicity).
- Appearance: It is striated, similar to skeletal muscle, due to the organized arrangement of contractile proteins.
- Energy Needs: Extremely high metabolic demand, with abundant mitochondria, and relies almost exclusively on aerobic respiration.

Microscopic Organization (Cardiomyocyte)
Cardiac muscle cells, or cardiomyocytes, are highly specialized cells with several unique features.
The Defining Feature: Intercalated Discs
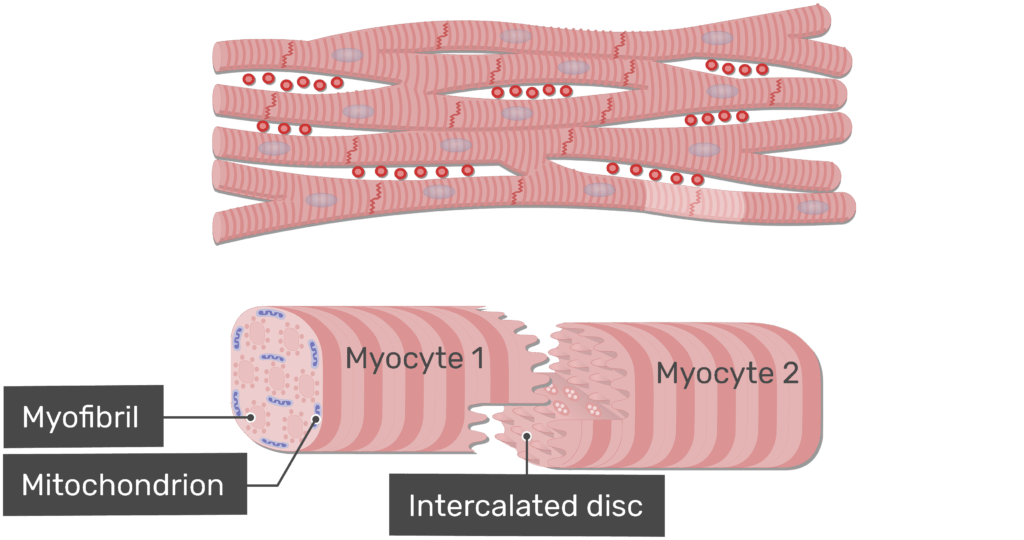
These are complex, specialized junctions that connect adjacent cardiomyocytes end-to-end, appearing as dark, wavy lines. They contain two vital components:
- Desmosomes: Act as strong anchoring points, preventing cells from separating during powerful contractions.
- Gap Junctions: Channels that allow electrical impulses to pass directly from cell to cell, ensuring the entire heart muscle contracts as a coordinated unit (a functional syncytium).
Other Microscopic Features:
- Cell Shape & Nuclei: Cells are shorter, thicker, and branched. Most contain a single, large, centrally located nucleus.
- Sarcoplasmic Reticulum (SR): Less extensive than in skeletal muscle. Cardiac muscle relies on both the SR and extracellular calcium to trigger contraction.
- Myofibrils & Sarcomeres: Contains organized myofibrils and sarcomeres, which produce the characteristic striations.
Mechanism of Contraction
Cardiac muscle contracts via the sliding filament model, but with key differences in initiation and regulation.
- Initiation (Autorhythmicity): Specialized pacemaker cells (e.g., in the SA node) spontaneously generate electrical impulses without nervous input. These impulses spread rapidly through the gap junctions.
- Calcium Handling: An initial influx of extracellular Ca²⁺ triggers the release of a larger amount of Ca²⁺ from the sarcoplasmic reticulum (calcium-induced calcium release).
- Long Refractory Period: Cardiac muscle has a long period where it cannot be re-stimulated. This is a critical safety feature that prevents tetanic (sustained) contractions, ensuring the heart has time to relax and refill with blood between beats.
Cardiac vs. Skeletal Muscle: Key Differences
| Feature | Skeletal Muscle | Cardiac Muscle |
|---|---|---|
| Control | Voluntary | Involuntary (autorhythmic) |
| Cell Shape | Long, cylindrical, unbranched | Shorter, branched |
| Nuclei | Many, peripheral | One or two, central |
| Intercalated Discs | Absent | Present (Desmosomes & Gap Junctions) |
| Ca²⁺ Source | Almost entirely from SR | SR + significant extracellular Ca²⁺ |
| Refractory Period | Short (can tetanus) | Long (prevents tetanus) |
| Mitochondria | ~2% of cell volume | 25-35% of cell volume |
Smooth Muscle Tissue
Smooth muscle is very distinct from skeletal and cardiac muscle. It is specialized for slow, sustained, involuntary contractions and is found in the walls of hollow internal organs (viscera). It performs many of the involuntary functions essential for life, such as digestion, blood pressure regulation, and elimination.
General Characteristics
- Location: Walls of hollow organs like the digestive tract, urinary bladder, reproductive tract, blood vessels, and respiratory airways.
- Function: Propulsion of substances (peristalsis), regulation of flow and pressure (vasoconstriction), and expulsion of contents (urination).
- Control: Involuntary. Regulated by the autonomic nervous system, hormones, and local chemical changes.
- Appearance: Non-striated, as its contractile proteins are not arranged in organized sarcomeres.

Microscopic Organization (Leiomyocyte)
Smooth muscle cells (leiomyocytes) are relatively simple in their morphology but have a sophisticated contractile mechanism.
Key Microscopic Features
- Spindle-shaped Cells: Elongated cells, widest in the middle and tapering to pointed ends, each with a single, centrally located nucleus.
- No Sarcomeres: Actin and myosin filaments are present but arranged diagonally in a lattice-like network, anchored by dense bodies (analogous to Z-discs).
- Calcium Source: The sarcoplasmic reticulum (SR) is much less developed. The majority of Ca²⁺ for contraction comes from the extracellular fluid.
- No Troponin: Instead of troponin, smooth muscle uses a protein called Calmodulin to bind Ca²⁺ and initiate contraction.
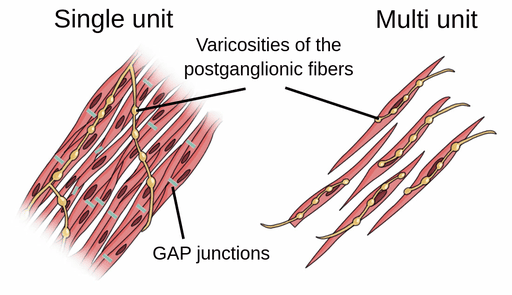
Types of Smooth Muscle
Smooth muscle is broadly categorized into two types based on its neural and functional characteristics:
1. Single-Unit (Visceral)
The most common type. Cells are electrically coupled by numerous gap junctions and contract rhythmically as a single unit (functional syncytium). Found in the walls of most hollow organs.
2. Multi-Unit
Consists of individual, structurally independent cells with few or no gap junctions. Each cell has its own nerve ending, allowing for fine, precise control. Found in large airways, large arteries, and the iris of the eye.
Smooth vs. Striated Muscle: Key Differences
| Feature | Striated Muscle (Skeletal/Cardiac) | Smooth Muscle |
|---|---|---|
| Striations | Yes (due to sarcomeres) | No (no sarcomeres) |
| Control | Voluntary (Skel), Involuntary (Card) | Involuntary |
| Cell Shape | Long, cylindrical/branched | Spindle-shaped |
| Troponin | Present (binds Ca²⁺) | Absent (Calmodulin binds Ca²⁺) |
| Ca²⁺ Source | Primarily SR (Skel), SR + ECF (Card) | Primarily Extracellular Fluid (ECF) |
| Contraction Speed | Fast, rapid | Slow, prolonged |
| Fatigue Resistance | Moderate (Skel), High (Card) | Very High |
Test Your Knowledge
Check your understanding of the concepts covered in this post.
1. Which type of muscular tissue is characterized by striations, multinucleated cells, and voluntary control?
- Smooth muscle
- Cardiac muscle
- Skeletal muscle
- All muscle types
2. The ability of muscle tissue to shorten forcibly when adequately stimulated is called:
- Excitability
- Extensibility
- Contractility
- Elasticity
3. Intercalated discs are a unique feature found in which type of muscular tissue?
- Skeletal muscle
- Smooth muscle
- Cardiac muscle
- Both skeletal and cardiac muscle
4. Which muscular tissue type is primarily responsible for peristalsis in the digestive tract?
- Skeletal muscle
- Cardiac muscle
- Smooth muscle
- Both skeletal and smooth muscle
5. What is the primary role of the sarcoplasmic reticulum in muscle contraction?
- Generating ATP
- Storing calcium ions (Ca2+)
- Producing neurotransmitters
- Providing elasticity to the muscle fiber
6. Which of the following statements about smooth muscle is TRUE?
- It has a rapid, powerful contraction.
- It contains highly organized sarcomeres.
- It is under involuntary control.
- It fatigues quickly.
7. The regulatory protein that binds calcium in skeletal and cardiac muscle is:
- Calmodulin
- Myosin
- Troponin
- Actin
8. Which type of muscular tissue would you expect to find in the walls of the urinary bladder and blood vessels?
- Skeletal muscle
- Cardiac muscle
- Smooth muscle
- Both skeletal and cardiac muscle
9. What is the function of the T-tubules in skeletal and cardiac muscle?
- To store glycogen for energy.
- To transmit the action potential deep into the muscle fiber.
- To synthesize contractile proteins.
- To produce new muscle cells.
10. A key difference in the initiation of contraction for smooth muscle compared to skeletal muscle is that smooth muscle uses primarily Ca2+ from:
- The sarcoplasmic reticulum only.
- Extracellular fluid and binds it to calmodulin.
- Intracellular fluid and binds it to troponin.
- The synaptic cleft.
11. The specialized plasma membrane of a muscle cell is called the _____________.
12. The functional unit of contraction in skeletal and cardiac muscle, characterized by a highly organized arrangement of myofilaments, is the _____________.
13. In cardiac muscle, gap junctions and desmosomes are found within specialized structures called ______________, which allow for rapid electrical communication and strong adhesion between cells.
14. The ability of a muscle cell to return to its original length after being stretched or contracted is known as _____________.
15. Smooth muscle cells are typically spindle-shaped and contain a single, centrally located _____________.
Quiz Complete!
Your Score:
0%
0 / 0 correct