Musculoskeletal System Anatomy: The Supporters.
Introduction to the Musculoskeletal System
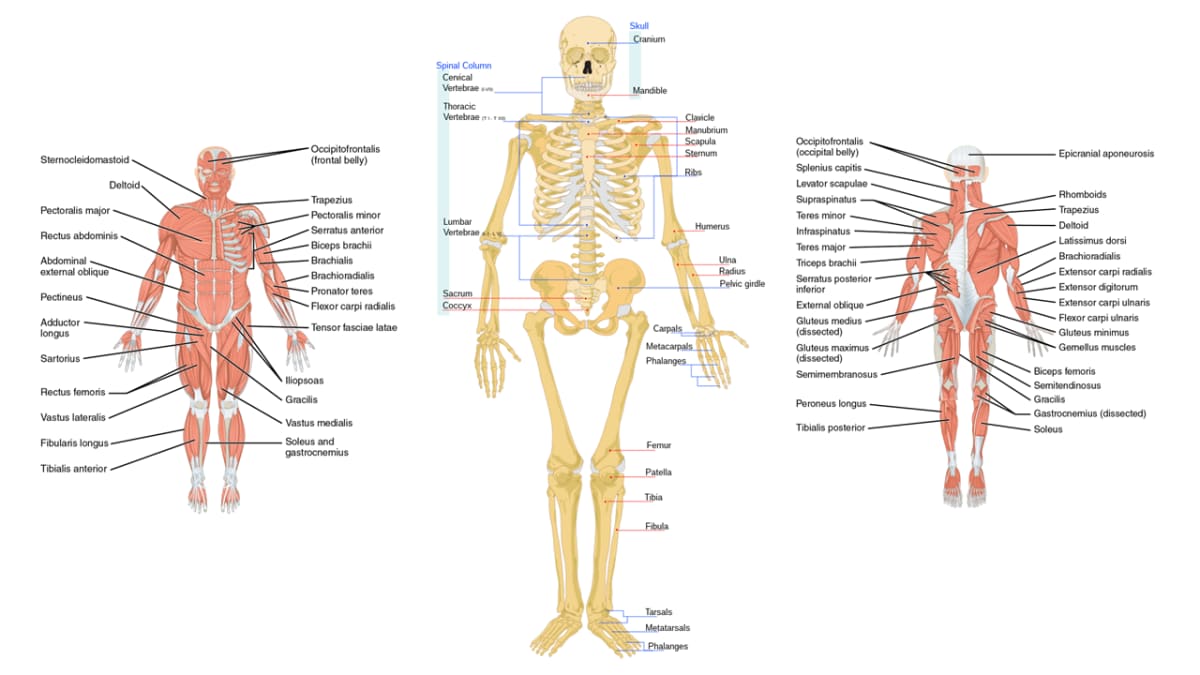
The Human Skeletal system is the body system composed of bones, cartilage, tendons, and ligaments and other tissues that perform essential functions for the human body. Altogether, the skeleton makes up about 20% of a person's body weight.
Components of the Musculoskeletal System
1. Bones
The rigid organs that form the body's structural framework. The human skeleton is composed of around 270 bones at birth, The adult human skeleton is composed of about 206 bones, which are made of specialized connective tissue with a mineralized matrix.
2. Cartilage
A soft, gel-like connective tissue that protects joints, facilitates smooth movement, and provides flexible support in areas like the nose, ears, and trachea.
3. Ligaments
Strong, tough bands of elastic connective tissue that connect bone to bone. They support and strengthen joints, limiting their movement to prevent injury. The body has approximately 900 ligaments.
4. Tendons
Strong, fibrous bands of connective tissue that attach muscle to bone. They transmit the force generated by muscle contractions to produce movement. The body has approximately 4,000 tendons.
5. Muscles (Skeletal)
Specialized contractile tissue attached to bones via tendons. Their voluntary contraction generates the force required for all conscious movement. The body has about 650 skeletal muscles.
Functions of the Musculoskeletal System
The coordinated action of these components provides the body with several critical functions.
Support
The skeleton forms the rigid internal framework that supports the body's weight and provides its shape.
Movement
Bones act as levers and muscles provide the force, allowing for locomotion and manipulation.
Protection
The skeleton safeguards vital internal organs (e.g., skull protects the brain, rib cage protects heart and lungs).
Mineral Storage
Bones act as a critical reservoir for essential minerals like calcium and phosphate.
Hematopoiesis
Red bone marrow, found within certain bones, is responsible for producing all blood cells.
Fat Storage
Yellow bone marrow stores triglycerides (fat) as a source of energy.
The Structure of Bone
Bones are the basic unit of the human skeleton. Far from being static, they are highly vascular, living tissues that are continuously remodeled throughout life. A bone is a rigid organ that protects internal organs, produces blood cells, stores minerals, provides structural support, and enables mobility. It is composed chiefly of calcium phosphate and calcium carbonate, serving as a critical reservoir for calcium.
Composition of Bone
Bone tissue is a composite material, made of both organic and inorganic components that give it its unique properties.
Organic Components (~35%)
Composed of osteoid (unmineralized matrix), which includes Type I collagen fibers and ground substance.
Inorganic Components (~65%)
Primarily hydroxyapatite (a complex of calcium phosphate) and other mineral salts like magnesium and fluoride.
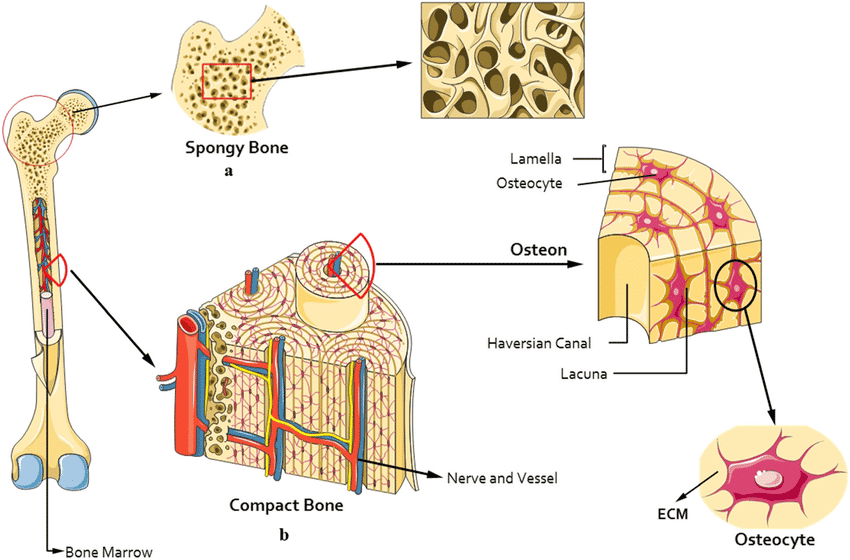
Types of Bone Tissue: Compact vs. Spongy
Bone has two main structural types, each with a distinct organization and function.
Compact Bone (Cortical Bone)
A dense, solid outer layer organized into repeating structural units called osteons (Haversian systems). Each osteon is a cylinder of concentric rings (lamellae) around a central Haversian canal, which contains blood vessels and nerves. This structure provides immense strength and protection, forming the outer layer of all bones and the shaft of long bones.
Spongy Bone (Cancellous Bone)
An internal, lightweight tissue that lacks osteons. It consists of an irregular latticework of thin columns of bone called trabeculae. The spaces between the trabeculae are filled with red bone marrow, the site of hematopoiesis. This structure provides strength without excessive weight and is found in the ends of long bones and in flat bones.
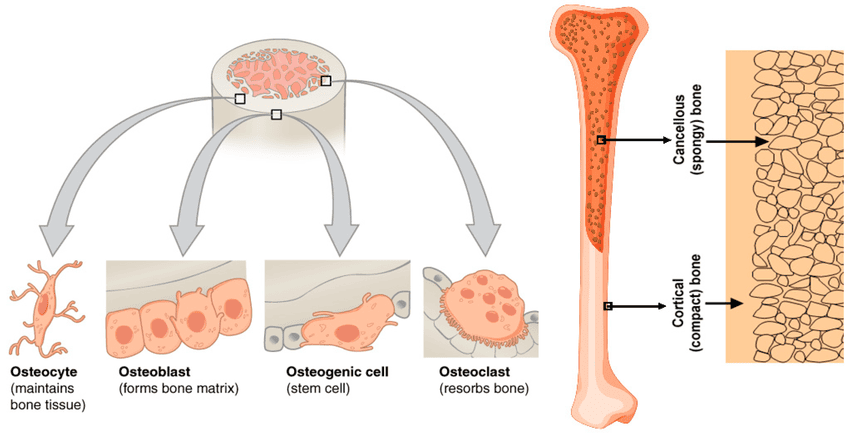
The Four Types of Bone Cells
Bone is a dynamic tissue maintained by four specialized cell types.
Osteogenic Cells
Function: Mesenchymal stem cells that divide and differentiate into osteoblasts. Crucial for bone growth and repair.
Osteoblasts
Function: Bone-building cells. They synthesize and secrete the organic osteoid matrix and initiate its calcification.
Osteocytes
Function: Mature, bone-maintaining cells trapped within the matrix. They act as mechanosensors, signaling for remodeling.
Osteoclasts
Function: Bone-resorbing cells. They break down bone matrix, which is essential for remodeling and releasing minerals into the blood.
The Gross Anatomy of Bone
Now that we've explored bone at the microscopic level, let's examine its larger, more observable features, including its classification, overall structure, and the critical bone markings that indicate interaction points with other body structures.
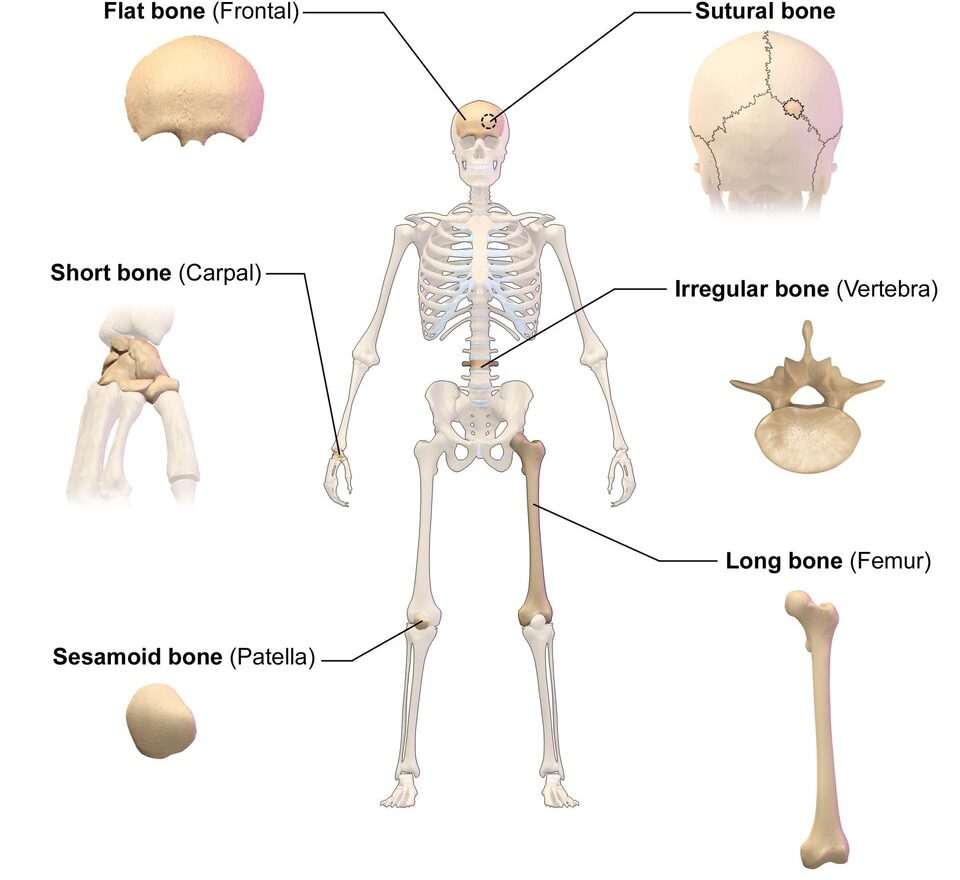
A. Classification of Bones by Shape
Long Bones
Longer than they are wide; act as levers for movement. (e.g., Femur, Humerus, Phalanges)
Short Bones
Cube-shaped; provide stability. (e.g., Carpals, Tarsals)
Flat Bones
Thin, flattened, and often curved; provide protection. (e.g., Cranial bones, Sternum, Ribs)
Irregular Bones
Complex and varied shapes. (e.g., Vertebrae, Hip bones)
Sesamoid Bones
Small bones embedded within tendons; protect tendons from stress. (e.g., Patella)
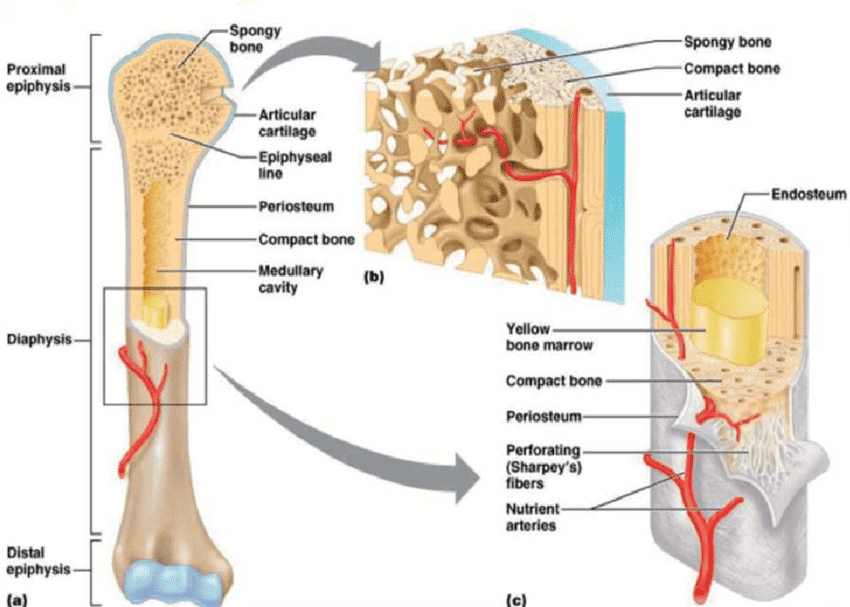
B. Structure of a Long Bone
Diaphysis
The main, cylindrical shaft of the bone, composed of compact bone surrounding the medullary cavity.
Epiphysis
The expanded ends of a long bone, consisting mostly of spongy bone.
Metaphysis
The region where the diaphysis and epiphysis meet. Contains the epiphyseal (growth) plate.
Articular Cartilage
A thin layer of hyaline cartilage covering the epiphysis at a joint to reduce friction.
Periosteum & Endosteum
The periosteum is the tough outer membrane, while the endosteum is the thin inner lining of the medullary cavity.
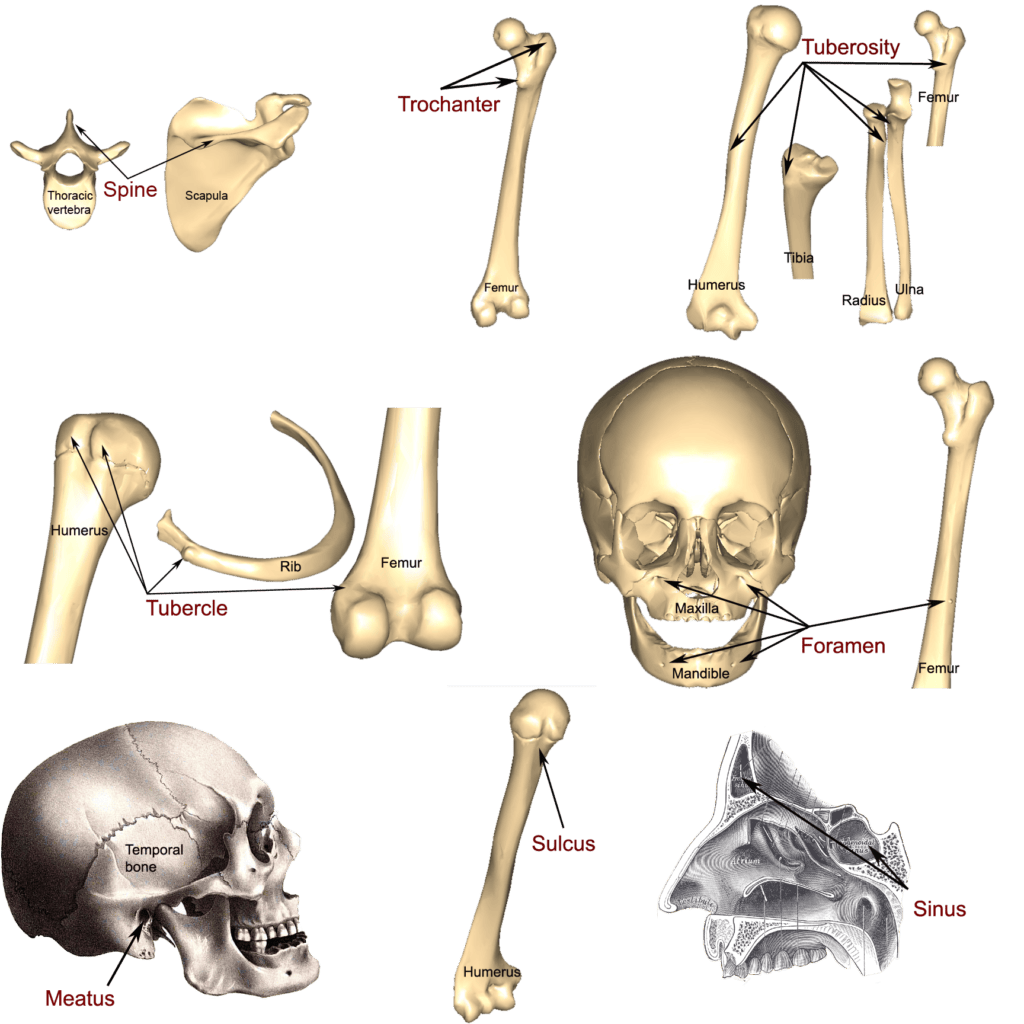
C. Bone Markings (Surface Features)
Bone markings are characteristic projections, depressions, and openings on bone surfaces that serve as points of articulation, attachment for muscles and ligaments, or passageways for nerves and blood vessels.
1. Projections (Features that Bulge Outward)
| Marking | Description | Example |
|---|---|---|
| Head | Prominent, rounded articular surface | Head of femur, Head of humerus |
| Condyle | Rounded articular projection | Femoral condyles |
| Epicondyle | Raised area above a condyle | Medial epicondyle of humerus |
| Process | Any bony prominence | Mastoid process |
| Spine | Sharp, slender projection | Ischial spine |
| Tubercle | Small, rounded projection | Tubercle of humerus |
| Tuberosity | Large, rounded, roughened projection | Deltoid tuberosity |
| Trochanter | Very large, blunt process (only on femur) | Greater trochanter |
| Crest | Narrow, prominent ridge of bone | Iliac crest |
| Line | Slight, elongated ridge | Temporal lines |
| Ramus | Arm-like bar of bone | Ramus of mandible |
2. Depressions and Openings (Indentations or Holes)
| Marking | Description | Example |
|---|---|---|
| Fossa | Shallow, basin-like depression | Mandibular fossa |
| Fovea | Small pit | Fovea capitis |
| Sulcus (Groove) | A channel-like depression | Intertubercular sulcus |
| Foramen | Round or oval hole through bone | Foramen magnum |
| Meatus | Canal-like passageway | External auditory meatus |
| Fissure | Narrow, slit-like opening | Superior orbital fissure |
| Sinus | Air-filled cavity within a bone | Paranasal sinuses |
| Facet | Smooth, nearly flat articular surface | Articular facets of vertebrae |
Bone Formation (Ossification)
Ossification, also known as osteogenesis, is the remarkable biological process of creating new bone tissue. All bone tissue originates from mesenchyme, a specialized embryonic connective tissue derived from the mesoderm. Mesenchymal stem cells can differentiate into both chondroblasts (cartilage-formers) and osteoblasts (bone-builders).
The Two Strategies for Bone Formation
The body employs two distinct methods to construct the skeleton, differing in their initial steps.
1. Intramembranous Ossification
Process: The simpler, more direct method where bone is formed directly within a sheet or "membrane" of mesenchymal tissue. No cartilage template is used.
Forms: Primarily the flat bones of the skull and face, and parts of the clavicle.
2. Endochondral Ossification
Process: A more complex, indirect method. A model made of hyaline cartilage is created first, which then serves as a scaffold that is systematically replaced by bone tissue.
Forms: Almost all other bones, including long bones, vertebrae, and ribs.
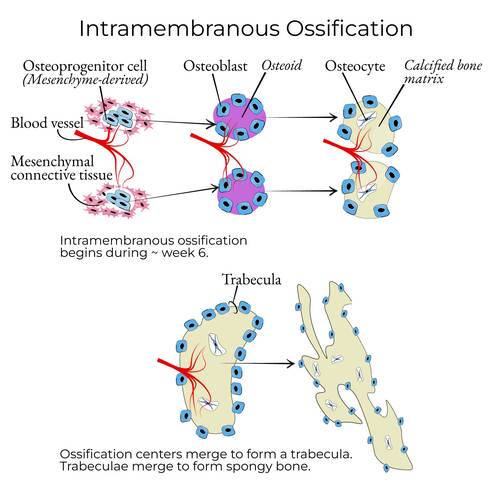
Intramembranous Ossification: A Step-by-Step Guide
This process occurs during fetal development and continues into infancy, forming the flat bones of the skull.
Step 1: Mesenchymal Cells Condense
In the precise location where a new bone is needed, mesenchymal stem cells begin to cluster closely together, signaling the start of bone formation.
"First, all the mesenchymal stem cells get a text message: 'Party at the skull-in-progress! Be there!' So they all cluster together in one spot."
Step 2: Differentiation and Osteoid Secretion
These clustered cells transform into osteoblasts, forming an ossification center. They immediately begin secreting osteoid, the unmineralized, organic matrix (mostly collagen) that acts as the soft framework for the bone.
"These cells change jobs. They become our bone-builders, the Osteoblasts. And what do they do? They start secreting this gooey stuff called osteoid. Think of it as the rebar and mesh before you pour the concrete."
Step 3: Calcification and Trapping of Osteocytes
Calcium salts are deposited into the osteoid, making it hard and rigid (calcification). Some osteoblasts become completely surrounded by the calcified matrix, getting trapped in small spaces called lacunae. Once trapped, they mature into osteocytes, which maintain the bone tissue.
"Now the concrete truck arrives! Calcium hardens that osteoid. Some of the osteoblast workers are a bit slow and get trapped in their own concrete! They just change jobs again and become Osteocytes—the site managers."
Step 4: Formation of Spongy Bone
The ossification process radiates outward, forming tiny, interconnected rods of bone called trabeculae. This creates the characteristic structure of spongy (cancellous) bone. Blood vessels weave through the spaces, and the remaining mesenchymal cells in these spaces differentiate into red bone marrow.
"This process keeps spreading out, creating a network of tiny bone struts called trabeculae. It looks like a sponge, which is why we call it spongy bone. Blood vessels sneak into the gaps, and the leftover mesenchyme turns into red bone marrow."
Step 5: Formation of Compact Bone and Periosteum
The surrounding mesenchyme condenses to form the periosteum, a protective outer membrane. The spongy bone just deep to the periosteum is then remodeled into a dense, strong layer of compact bone, creating a "sandwich" structure with spongy bone in the middle.
"Finally, the mesenchyme on the outside forms a tough wrapper called the periosteum. The spongy bone right underneath gets remodeled into super-dense compact bone. So you end up with a bone sandwich: two layers of hard compact bone with a spongy, marrow-filled center."
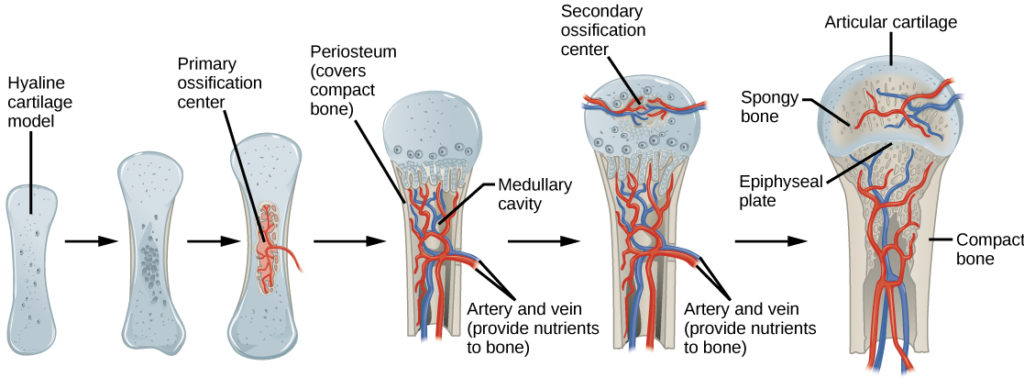
Endochondral Ossification: Building on a Cartilage Model
This more intricate process is responsible for the formation and longitudinal growth of most bones in the body, particularly the long bones. It uses a hyaline cartilage model as a precursor.
Step 1: The Hyaline Cartilage Model is Formed
Mesenchymal cells differentiate into chondroblasts, which produce a miniature, scaled-down model of the future bone made entirely of hyaline cartilage, surrounded by a perichondrium.
"First, the body makes a perfect, wobbly model of the bone out of hyaline cartilage. It’s the exact shape of the final bone, just… squishier."
Step 2: Hypertrophy and Calcification in the Center
In the center of the diaphysis, chondrocytes swell (hypertrophy) and cause the surrounding cartilage matrix to calcify, making it rigid.
"The cartilage cells right in the middle of the shaft get big and swollen. They get so big they make the area around them hard and chalky. It calcifies."
Step 3: The Periosteal Bone Collar Forms (Primary Ossification Center)
The perichondrium transforms into the periosteum. Osteoblasts in its inner layer secrete a thin layer of bone around the diaphysis, called the subperiosteal bone collar. This marks the establishment of the primary ossification center.
"The outer wrapping sees what’s happening and turns into a periosteum. Its osteoblasts build a thin collar of bone around the middle of the shaft. This is our primary ossification center."
Step 4: Invasion of the Osteogenic Bud
The calcified cartilage matrix blocks nutrient diffusion, causing the central chondrocytes to die and leaving empty cavities. An osteogenic bud (a blood vessel with osteoprogenitor cells and osteoclasts) invades these central cavities.
"The cartilage cells in the middle can't get any food, and they die. Then, the cavalry arrives! A blood vessel called the osteogenic bud drills its way in, bringing the Osteoclasts (demolition team) and more Osteoblasts (construction team)."
Step 5 & 6: Spongy Bone Formation and Medullary Cavity
Osteoclasts break down the dead cartilage, while osteoblasts lay down new bone matrix on the remnants, forming spongy bone. As this ossification center expands towards the ends of the bone, osteoclasts in the very center resorb the newly formed bone, carving out the medullary (marrow) cavity.
"The osteoclasts clear out the dead cartilage, and the osteoblasts build spongy bone. The demolition crew is very efficient, hollowing out the very center of the shaft to create the medullary cavity. It’s a constant cycle of building and carving."
Step 7: Secondary Ossification Centers Appear
After birth, a similar process occurs in the epiphyses (the ends of the bone). Blood vessels invade the cartilage ends, and spongy bone is formed, creating secondary ossification centers. This transforms the cartilage ends into bone, though some articular cartilage remains.
"After the baby is born, this whole process starts all over again at the ends of the bone, the epiphyses. These are the secondary ossification centers."
How Bones Grow in Length (Longitudinal Growth)
The continuous increase in the length of long bones is driven by the epiphyseal growth plate, a thin layer of hyaline cartilage between the diaphysis and each epiphysis. This plate is organized into distinct zones:
- Zone of Reserve Cartilage: Anchors the growth plate to the epiphysis.
- Zone of Proliferation: Chondrocytes undergo rapid mitosis, forming stacks of new cells that push the epiphysis away from the diaphysis, adding length.
- Zone of Hypertrophy & Maturation: Chondrocytes stop dividing and enlarge significantly.
- Zone of Calcification: The surrounding matrix calcifies, and the chondrocytes die.
- Zone of Ossification: Osteoclasts remove the dead cartilage, and osteoblasts lay down new bone on the remaining scaffolding, extending the diaphysis.
At the end of puberty, hormonal changes cause this cartilage growth to stop. The plate is completely replaced by bone, leaving a faint epiphyseal line, and longitudinal growth ceases.
How Bones Grow in Width (Appositional Growth)
Bones also grow in width to become thicker and stronger through appositional growth. This is a balanced process:
- On the Outside: Osteoblasts in the periosteum deposit new layers of bone onto the outer surface, increasing the bone's diameter.
- On the Inside: Simultaneously, osteoclasts in the endosteum resorb bone from the inner surface that lines the medullary cavity.
This coordinated action allows the bone to increase in diameter and strength without becoming excessively dense and heavy.
Bone Healing (Fracture Repair)
Bone healing is a remarkable biological process that follows a predictable sequence of events to restore the integrity of a broken bone. Unlike soft tissue repair, which often results in scar tissue, bone healing has the unique ability to restore the original bone structure.
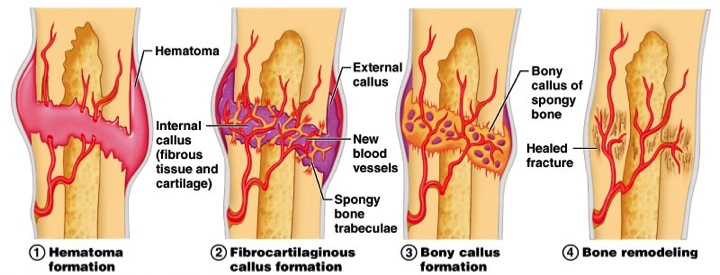
The Four Stages of Fracture Repair
Stage 1: Hematoma Formation (Inflammatory Stage)
Immediately after a fracture, torn blood vessels hemorrhage, forming a mass of clotted blood called a hematoma at the fracture site. The area becomes swollen and inflamed, and bone cells deprived of nutrition die. Phagocytic cells and osteoclasts begin to clean up the debris.
Stage 2: Fibrocartilaginous Callus Formation (Soft Callus)
Within days to weeks, new capillaries grow into the hematoma. Fibroblasts produce collagen fibers to connect the broken ends, while chondroblasts secrete a cartilage matrix. This entire mass of repair tissue is known as the fibrocartilaginous (soft) callus, which acts as a natural splint for the bone ends.
Stage 3: Bony Callus Formation (Hard Callus)
Over weeks to months, osteoblasts become active and gradually convert the soft callus into a hard, bony callus of spongy bone. This process firmly unites the two bone fragments, significantly increasing the strength of the repair site.
Stage 4: Bone Remodeling
Over several months to years, the bony callus is remodeled. Osteoclasts remove excess material on the outside of the bone and within the medullary cavity. Osteoblasts lay down compact bone to reconstruct the shaft walls. This final phase restores the bone to its original shape and strength, often leaving little to no trace of the original injury.
Factors Influencing Bone Healing
The success and speed of fracture repair can be influenced by a variety of local and systemic factors.
- Fracture Severity and Type: Simple fractures heal more quickly than complex, comminuted, or open (compound) fractures.
- Blood Supply: An adequate blood supply is absolutely crucial for delivering the necessary cells, oxygen, and nutrients to the fracture site.
- Immobilization: Proper alignment and stabilization (e.g., with a cast or surgical fixation) are essential to prevent movement that could disrupt the delicate callus.
- Nutrition: A diet rich in calcium, vitamin D, vitamin C (for collagen synthesis), and protein is vital for building new bone.
- Age: Children and adolescents generally heal much faster than adults and the elderly.
- Health Status: Chronic diseases (like diabetes), systemic infections, and certain medications (e.g., corticosteroids) can significantly impair or delay the healing process.
- Hormones: Growth hormone, thyroid hormones, and hormones that regulate calcium (calcitonin, parathyroid hormone) all play important roles in bone metabolism and repair.
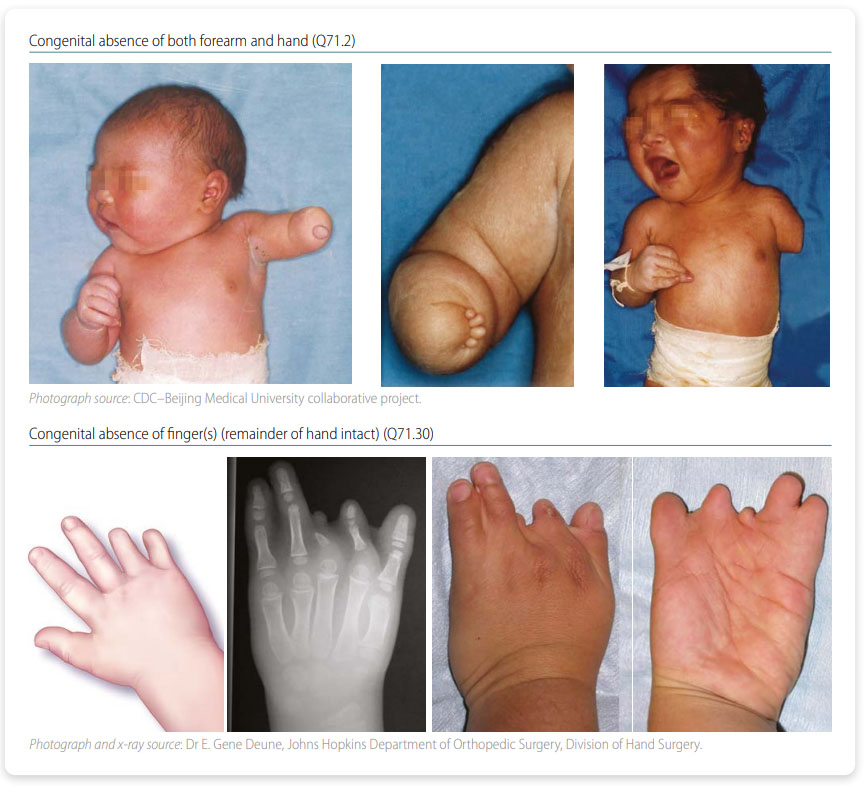
Congenital Bone Malformations
Congenital bone malformations, also known as skeletal dysplasias, are a group of over 400 rare genetic disorders that affect the development of bones and cartilage. These conditions result in abnormalities in the size and shape of the skeleton, affecting approximately 1 in every 5,000 births.
I. Disorders of Bone Formation (Dysplasias)
These involve abnormal development of bone or cartilage tissue itself, leading to generalized skeletal defects.
Achondroplasia
Description: The most common form of short-limbed dwarfism, caused by a mutation in the FGFR3 gene that impairs cartilage formation, leading to severely shortened long bones.
Osteogenesis Imperfecta (Brittle Bone Disease)
Description: A group of genetic disorders characterized by extremely fragile bones that break easily, caused by defects in Type I collagen production. Features include frequent fractures, blue sclera, and hearing loss.
II. Disorders of Bone Number or Fusion
These involve having too many, too few, or improperly fused bones.
Polydactyly & Syndactyly
Polydactyly is the presence of extra fingers or toes. Syndactyly is the fusion of two or more digits ("webbed" fingers/toes).
Spina Bifida
Description: A neural tube defect where the vertebral arches fail to fuse posteriorly. Severity ranges from mild (occulta) to severe (myelomeningocele), where the spinal cord protrudes.
Craniosynostosis
Description: The premature fusion of one or more cranial sutures in an infant's skull, leading to an abnormally shaped head and restricted brain growth.
III. Disorders of Limb Development
These involve malformations of the entire limb or significant portions of it.
Amelia
Description: The complete absence of an arm or leg, resulting from a severe disruption of early limb bud development.
Phocomelia
Description: A condition where the hands or feet are attached close to the trunk, with the limbs being greatly reduced in size or absent. Notably associated with thalidomide exposure.
IV. Genetic Syndromes with Skeletal Manifestations
Many genetic syndromes include skeletal abnormalities as part of their broader clinical picture.
Marfan Syndrome
Description: A connective tissue disorder caused by a mutation in the FBN1 gene. Skeletal features include tall stature, long limbs and fingers (arachnodactyly), flexible joints, scoliosis, and chest deformities.
Test Your Knowledge
Check your understanding of the Skeletal System's structure and function.
1. Which of the following is NOT a primary function of the skeletal system?
- Support and protection
- Mineral storage
- Blood cell formation
- Hormone production
Correct (d): While some endocrine functions are associated with bone (e.g., osteocalcin), hormone production is not considered a primary function of the skeletal system itself in the same way as support, protection, mineral storage, or hematopoiesis.
Incorrect (a): The skeleton provides the body's framework (support) and encases vital organs like the brain and spinal cord (protection).
Incorrect (b): Bones serve as a reservoir for calcium, phosphate, and other essential minerals.
Incorrect (c): Red bone marrow, found within certain bones, is the primary site of hematopoiesis (blood cell formation).
2. Which type of bone cell is responsible for breaking down bone tissue?
- Osteoblast
- Osteocyte
- Osteoclast
- Chondrocyte
Correct (c): Osteoclasts are large, multinucleated cells derived from monocytes that resorb (break down) bone tissue, releasing minerals into the blood.
Incorrect (a): Osteoblasts are bone-forming cells that synthesize and deposit new bone matrix.
Incorrect (b): Osteocytes are mature bone cells, trapped within the bone matrix, that maintain bone tissue.
Incorrect (d): Chondrocytes are cells found in cartilage, not directly involved in bone tissue breakdown.
3. The process of bone formation from a cartilaginous model is called:
- Intramembranous ossification
- Endochondral ossification
- Appositional growth
- Interstitial growth
Correct (b): Endochondral ossification is the process where bone develops by replacing a hyaline cartilage model. Most bones of the body, especially long bones, form this way.
Incorrect (a): Intramembranous ossification is the direct formation of bone from mesenchymal connective tissue, primarily forming flat bones.
Incorrect (c): Appositional growth refers to the increase in bone width.
Incorrect (d): Interstitial growth refers to the increase in length of cartilage or bone from within.
4. Which zone of the epiphyseal plate is responsible for the proliferation of chondrocytes, leading to longitudinal bone growth?
- Zone of resting cartilage
- Zone of proliferation
- Zone of hypertrophy
- Zone of calcification
Correct (b): In the zone of proliferation, chondrocytes rapidly divide by mitosis, pushing the epiphysis away from the diaphysis and lengthening the bone.
Incorrect (a): The zone of resting cartilage anchors the epiphyseal plate to the epiphysis.
Incorrect (c): In the zone of hypertrophy, chondrocytes enlarge and mature.
Incorrect (d): In the zone of calcification, the cartilage matrix calcifies, and the chondrocytes die.
5. Which of the following is the final stage of bone repair after a fracture?
- Hematoma formation
- Fibrocartilaginous callus formation
- Bony callus formation
- Bone remodeling
Correct (d): Bone remodeling is the long-term process where the bony callus is reshaped and strengthened by osteoblasts and osteoclasts, eventually restoring the original bone structure.
Incorrect (a): Hematoma formation is the initial stage.
Incorrect (b): Fibrocartilaginous callus formation is the second stage.
Incorrect (c): Bony callus formation is the third stage, preceding remodeling.
6. Which classification of bone is primarily composed of trabeculae and contains red bone marrow?
- Compact bone
- Cortical bone
- Spongy bone
- Lamellar bone
Correct (c): Spongy (cancellous) bone is characterized by a network of bony struts called trabeculae, which provide strength with minimal weight and house red bone marrow.
Incorrect (a) & (b): Compact (cortical) bone is the dense, solid outer layer of bones.
Incorrect (d): Lamellar bone is a structural term for mature bone tissue, which can be either compact or spongy.
7. Which hormone plays a crucial role in regulating blood calcium levels by stimulating osteoclast activity?
- Calcitonin
- Growth hormone
- Parathyroid hormone (PTH)
- Thyroid hormone
Correct (c): Parathyroid hormone (PTH) is released when blood calcium levels are low. It stimulates osteoclasts to resorb bone, releasing calcium into the bloodstream.
Incorrect (a): Calcitonin is released when blood calcium levels are high and inhibits osteoclast activity.
Incorrect (b): Growth hormone promotes overall bone growth but does not primarily regulate acute calcium levels.
Incorrect (d): Thyroid hormone influences metabolic rate but is not the primary regulator of blood calcium.
8. The term for a break in a bone is a:
- Sprain
- Strain
- Fracture
- Dislocation
Correct (c): A fracture is specifically a break or crack in a bone.
Incorrect (a): A sprain is an injury to ligaments (tissue connecting bones to bones).
Incorrect (b): A strain is an injury to a muscle or tendon (tissue connecting muscle to bone).
Incorrect (d): A dislocation occurs when bones at a joint are forced out of alignment.
9. Which of the following bone cells are considered "bone-forming" cells?
- Osteocytes
- Osteoclasts
- Osteoblasts
- Chondroblasts
Correct (c): Osteoblasts are responsible for synthesizing and secreting the organic components of the bone matrix and initiating its mineralization, thus building new bone.
Incorrect (a): Osteocytes are mature bone cells that maintain the bone matrix.
Incorrect (b): Osteoclasts are bone-resorbing cells.
Incorrect (d): Chondroblasts are cells that form cartilage, not bone.
10. The process of bone remodeling involves the continuous coordinated activity of:
- Osteoblasts and chondrocytes
- Osteoclasts and chondrocytes
- Osteoblasts and osteoclasts
- Osteocytes and fibroblasts
Correct (c): Bone remodeling is a dynamic process where old bone is continuously removed by osteoclasts (resorption) and replaced by new bone formed by osteoblasts (formation).
Incorrect (a) & (b): Chondrocytes are primarily involved in cartilage formation, not the ongoing remodeling of mature bone.
Incorrect (d): Fibroblasts produce connective tissue but are not the primary cells of bone remodeling.
11. The shaft of a long bone is called the _____________.
12. The inorganic matrix of bone is primarily composed of mineral salts, mainly _____________.
13. The growth plate in long bones, responsible for increasing bone length, is known as the _____________ plate.
14. The specialized connective tissue that lines the medullary cavity and covers the trabeculae of spongy bone is the _____________.
15. A complete break in a bone where the bone ends penetrate the skin is called a _____________ fracture.
Quiz Complete!
Your Score:
0%
0 / 0 correct