GIT Secretions
Gastrointestinal (GIT) Secretions
The gastrointestinal tract is equipped with a diverse array of secretory glands that play two fundamental roles:
- Secretion of Digestive Enzymes: These enzymes are essential for breaking down complex food molecules into absorbable units. This enzymatic activity occurs from the mouth all the way to the distal end of the ileum.
- Provision of Mucus: Mucus serves as a lubricant and protective barrier for the entire GIT, from the mouth to the anus.
Key Principle: The presence of food in the GIT is the primary stimulus for secretions. The quantity and type of secretions are precisely regulated to match the amount and type of food present, ensuring efficient digestion.
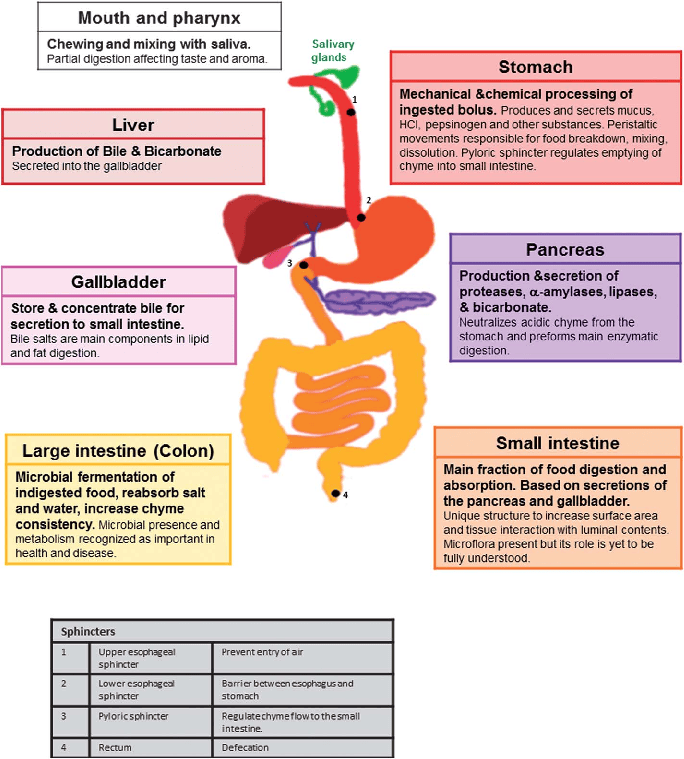
Anatomical Types of Glands in the GIT
The GIT houses several types of glands, each contributing to the overall secretory process:
- Goblet Cells/Simple Mucous Cells: These are single-celled glands interspersed among the epithelial cells. They directly extrude mucus onto the epithelial surface, providing immediate lubrication and protection. They are found throughout the GIT.
- Crypts of Lieberkühn: These are invaginations or pits found deep within the mucosa of the small intestine and large intestine. They contain various specialized secretory cells, including enterocytes (which secrete water and electrolytes), goblet cells, and enteroendocrine cells.
- Tubular Glands: These glands are typically found deeper within the mucosal layer.
- Stomach: Examples include the oxyntic glands (gastric glands) in the body and fundus, which secrete acid, pepsinogen, intrinsic factor, and mucus, and pyloric glands in the antrum, which secrete mucus and gastrin.
- Upper Duodenum: Brunner's glands, located in the submucosa of the duodenum, secrete alkaline mucus to protect against acidic chyme from the stomach.
- Complex Glands (Extramural Glands): These are large, accessory glands located outside the wall of the GIT but connected to it by ducts. They provide copious secretions crucial for digestion or emulsification.
- Salivary Glands: Produce saliva for initial digestion and lubrication.
- Pancreas: Secretes pancreatic juice containing a wide array of digestive enzymes and bicarbonate.
- Liver: Produces bile, essential for fat emulsification.
Mechanism of Secretion by Glandular Cells
Glandular cells in the GIT typically secrete two main types of substances simultaneously:
- Organic Substances: This includes digestive enzymes (proteins), mucin (glycoproteins), and hormones. These are synthesized within the cells and packaged into vesicles before exocytosis.
- Water and Electrolytes: These are secreted to create a fluid environment for the organic substances and to aid in transport and hydration. The movement of water and electrolytes is often regulated by ion pumps and channels, creating osmotic gradients.
Mucus: Properties and Role
Mucus is a vital secretion found throughout the GIT, acting as both a lubricant and a protectant.
- Composition: Mucus is a thick, viscous secretion primarily composed of water, electrolytes, and a mixture of several glycoproteins. These glycoproteins are large polysaccharides with smaller quantities of protein attached.
- Key Properties:
- Adherent Qualities: Mucus readily adheres to surfaces, forming a continuous coating.
- Coats the Gut Wall: It has sufficient "body" or viscosity to effectively coat and protect the entire luminal surface of the GIT.
- Low Resistance for Slippage: Provides a slippery surface, allowing food (bolus or chyme) to move easily along the tract without causing damage.
- Causes Fecal Particles to Adhere: In the large intestine, mucus helps bind fecal particles together, facilitating their smooth passage.
- Strongly Resistant to Digestion: Its complex structure and chemical properties make it highly resistant to breakdown by digestive enzymes, ensuring its protective function.
- Amphoteric Glycoproteins: The glycoproteins in mucus are amphoteric, meaning they can act as both an acid and a base. This property allows mucus to buffer against both acidic and alkaline conditions, protecting the underlying mucosa.
The 4 Main Secretions of the GIT
1. Saliva
Saliva is the first major digestive secretion, produced by the salivary glands in the mouth.
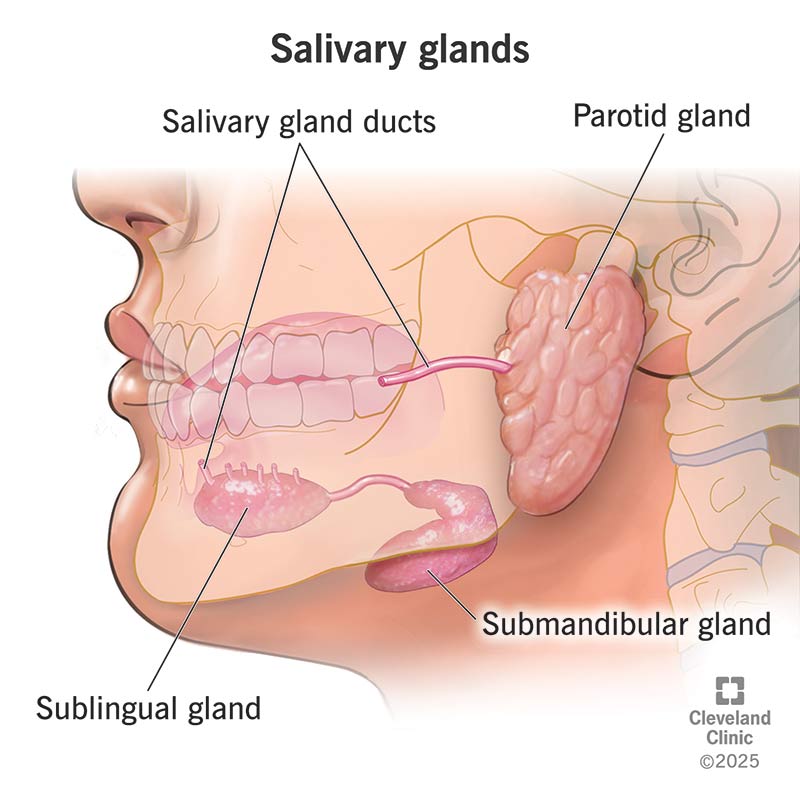
A. Salivary Glands
- Three Principal Glands (Major Salivary Glands):
- Parotid Glands: Largest salivary glands, located below and in front of the ears. They secrete entirely serous (watery, enzyme-rich) saliva.
- Submandibular Glands: Located under the floor of the mouth. They secrete a mixed serous and mucous saliva.
- Sublingual Glands: Smallest of the major glands, located under the tongue. They primarily secrete mucous saliva, with some serous component.
- Minor Salivary Glands: Numerous small buccal glands (and other minor glands throughout the oral cavity) secrete only mucus.
- Daily Secretion Volume: The total daily secretion of saliva ranges between 800 and 1500 ml, with an average of about 1000 ml.
B. Composition of Saliva
Saliva is a complex fluid containing two major types of protein secretions:
- Serous Secretion: A watery fluid containing digestive enzymes. The main enzyme is ptyalin (salivary α-amylase), which initiates carbohydrate digestion.
- Mucus Secretion: Contains mucin, a glycoprotein that provides lubrication.
pH of Saliva: Between 6.0 and 7.0, which is slightly acidic to neutral.
C. How Saliva is Secreted (Two-Stage Process)
Saliva is not a simple ultrafiltrate. Its composition is modified as it passes through the ducts. A typical submandibular gland, being a compound gland, illustrates this two-stage process:
- Primary Secretion by Acini:
- The acinar cells (the secretory units) produce a "primary secretion" that is roughly isotonic with plasma.
- This primary secretion contains ptyalin (α-amylase) and/or mucin, along with water and ions (similar to extracellular fluid).
- Modification in Salivary Ducts: As the primary secretion flows through the salivary ducts, significant changes occur:
- Sodium (Na+) Reabsorption: Na+ is actively reabsorbed from the ductal lumen into the interstitial fluid.
- Potassium (K+) Secretion: K+ is actively secreted from the interstitial fluid into the ductal lumen.
- Chloride (Cl-) Reabsorption: Cl- is reabsorbed passively, following Na+ due to the electrical gradient.
- Bicarbonate (HCO3-) Secretion: Bicarbonate ions are actively secreted by the ductal epithelium into the duct lumen.
Net Effect: The net reabsorption of Na+ and Cl- is greater than the secretion of K+ and HCO3-. This results in a hypotonic final saliva (more dilute than plasma), especially at lower flow rates.
D. Function of Saliva in Oral Hygiene
The mouth is constantly exposed to pathogenic bacteria and food particles. Saliva plays a crucial role in maintaining oral health:
- Washing Action: Saliva continuously washes away pathogenic bacteria and food particles, preventing their accumulation and subsequent growth.
- Antibacterial Factors: Contains several factors that actively destroy bacteria:
- Thiocyanates: An antimicrobial compound.
- Proteolytic Enzymes (Lysozyme): An enzyme that can lyse (break open) bacterial cell walls.
- Protein Antibodies: Contains IgA antibodies that can agglutinate or neutralize oral bacteria.
- Consequences of Saliva Absence: In the absence of adequate salivation (xerostomia), oral tissues become ulcerated and infected, and dental caries (tooth decay) can become rampant.
E. Nervous Regulation of Salivary Secretion
Salivary secretion is exclusively under nervous control; GI hormones do not directly regulate it. Both divisions of the autonomic nervous system stimulate salivation, though parasympathetic activity is dominant.
Parasympathetic Stimulation
- Primary Stimulus: Strongest stimulus for copious, watery saliva.
- Pathway: Fibers from the salivary nuclei in the brainstem (via facial and glossopharyngeal nerves).
- Neurotransmitter: Acetylcholine (ACh), acting on muscarinic receptors.
- Effects: Causes vasodilation (increased blood flow) and directly stimulates acinar/ductal cells to secrete a large volume of enzyme-rich, watery saliva.
Sympathetic Stimulation
- Secondary Stimulus: Generally produces a smaller volume of thicker, mucus-rich saliva.
- Pathway: Fibers originate from the upper thoracic spinal cord -> superior cervical ganglion.
- Neurotransmitter: Norepinephrine, acting on adrenergic receptors.
- Effects: Causes vasoconstriction and stimulates protein (mucin) secretion, leading to a more viscous saliva.
F. Salivation Pathophysiology
1. Hyposalivation
- Temporary Causes: Emotional conditions, Fever, Dehydration.
- Permanent Causes: Sialolithiasis (stone obstruction), Congenital absence, Bell's Palsy, Drugs (antihistamines, antidepressants), Sjögren's syndrome.
2. Hypersalivation (Ptyalism)
- Physiological: Pregnancy.
- Pathological: Dental issues, GI diseases (reflux, ulcers), Neurological disorders (Parkinson's, rabies), Psychological conditions, Nausea, Toxins (mercury).
3. Xerostomia ("Dry Mouth")
- Definition: Subjective feeling of dry mouth.
- Consequences: Difficulty mastication/swallowing/speech, Halitosis, Dental caries.
- Causes: Dehydration, Renal failure, Sjögren's Syndrome, Radiotherapy, Trauma, Drugs (antimuscarinic), Shock.
Esophageal Secretions
- Type of Secretion: Esophageal glands secrete almost entirely mucus.
- Purpose: Lubrication for bolus passage and protection of the wall.
- Specific Protective Roles:
- Upper Esophagus: Prevents mucosal excoriation by rough food.
- Esophagogastric Junction (Lower Esophagus): Protects from digestion by acidic gastric juices that reflux.
- Limitations: If reflux is severe/prolonged, a peptic ulcer can occur.
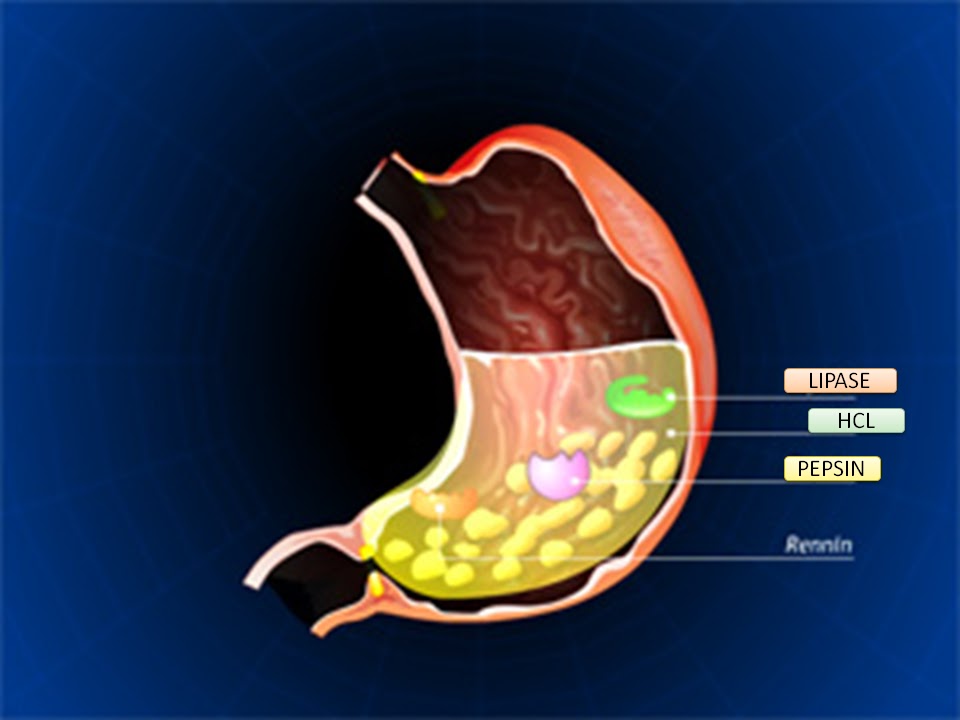
2. Gastric Juice: The Stomach's Digestive and Protective Secretion
Gastric juice is a highly acidic and enzyme-rich fluid secreted by glands in the stomach lining.
A. Gastric Glands
1. Oxyntic Glands (Gastric Glands)
Found in the body and fundus (80%).
- Mucous Neck Cells: Secrete mucus and some pepsinogen.
- Peptic (Chief) Cells: Secrete pepsinogen (precursor to pepsin).
- Parietal (Oxyntic) Cells: Secrete hydrochloric acid (HCl) and intrinsic factor (essential for Vit B12 absorption).
2. Pyloric Glands
Located in the antrum (20%).
- Few peptic cells, almost no parietal cells.
- Primarily mucous cells: Secrete thin mucus and some pepsinogen.
- G cells: Secrete the hormone gastrin.
Surface Mucous Cells: Cover the entire surface, producing thick, alkaline mucus as a protective barrier.
Stimulation of Gastric Acid (HCl) Secretion
HCl is secreted by parietal cells at pH ~0.8.
Key Regulators of Parietal Cells: Mediated via Enterochromaffin-like (ECL) cells.
- ECL Cells: Secrete histamine, which directly stimulates parietal cells to secrete HCl.
- Control of ECL Cells:
- Gastrin Hormone: Secreted by G cells. Most potent stimulator. Stimulates ECL cells to release histamine.
- Acetylcholine (ACh): From vagal nerve endings. Directly stimulates parietal, peptic, and ECL cells.
- Hormonal Substances from ENS: Contribute to regulation.
Regulation of Pepsinogen Secretion
- Neural Stimulation: ACh from vagus nerves/enteric plexus.
- Acid in the Stomach: Low pH triggers a positive feedback loop. Clinical Relevance: In achlorhydria, pepsinogen secretion is also markedly decreased.
Phases of Gastric Secretion
| Phase | % of Secretion | Stimuli & Mechanism |
|---|---|---|
| 1. Cephalic Phase | 30% | Stimuli: Sight, smell, taste, thought of food. Mechanism: Brain -> Vagus nerve -> Stimulates Parietal/Peptic/G cells. |
| 2. Gastric Phase | 60% | Stimuli: Food in stomach (distention). Mechanism: Local reflexes, Vagovagal reflexes, Gastrin-Histamine stimulation. (Most significant phase). |
| 3. Intestinal Phase | 10% | Stimuli: Chyme in duodenum. Mechanism: Initial small gastrin release, followed by strong inhibition. |
Inhibition of Gastric Secretion
To prevent the duodenum from being overwhelmed by acid:
- Reverse Enterogastric Reflex: Triggered by distention, acid, or fat in the small intestine. Inhibits stomach motility and secretion via nervous pathways.
- Intestinal Hormones (Enterogastrones): Released from duodenal/jejunal mucosa.
- Secretin: Released in response to acid. Inhibits gastric acid.
- Gastric Inhibitory Peptide (GIP): Released in response to fat/carbs.
- Somatostatin: Inhibits gastrin and HCl.
Gastric Pathophysiology
1. Gastritis
Acute: Superficial inflammation (NSAIDs, alcohol).
Chronic: Deeper inflammation (Helicobacter pylori, autoimmune). Can lead to atrophy.
2. Gastric Atrophy
Severe chronic gastritis. Muscles shrink, glands waste away.
Consequences:
- Achlorhydria: No HCl.
- Pernicious Anemia: Loss of intrinsic factor -> No Vit B12 absorption.
- Increased Cancer Risk.
3. Peptic Ulcer
Excoriated area of mucosa. Imbalance between aggressive factors (acid, pepsin, H. pylori) and defensive factors.
Treatment: Antibiotics (for H. pylori), PPIs (Omeprazole), H2 Blockers (Ranitidine).
4. Zollinger-Ellison Syndrome (ZES)
Excess HCl caused by a gastrinoma (gastrin-secreting tumor).
Symptoms: Severe pain, diarrhea (enzyme inactivation), ulcers.
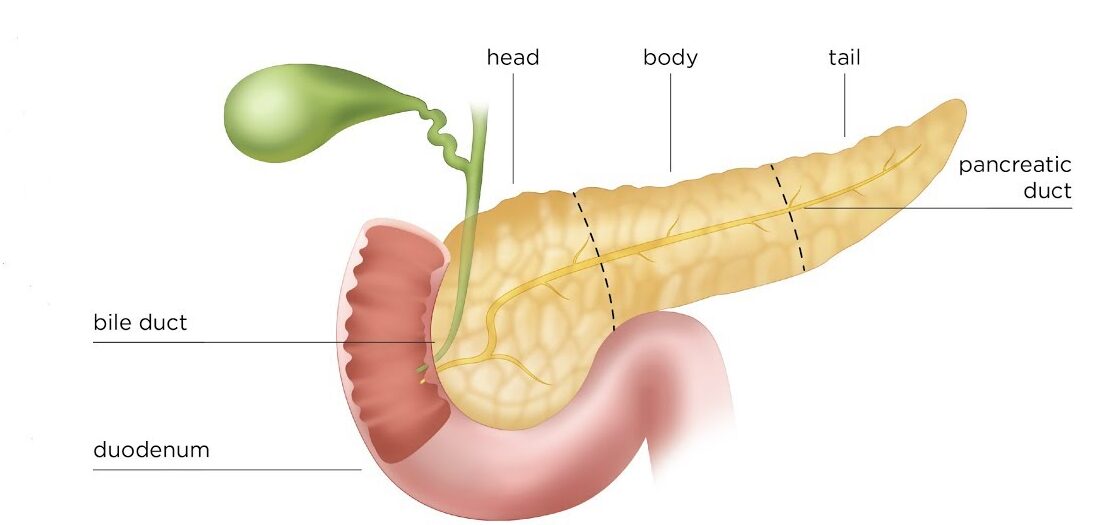
3. Pancreatic Juice
Secreted by the pancreas, a large compound gland.
A. Structure and Secretion
- Enzymes: Secreted by pancreatic acini.
- Bicarbonate (HCO3-): Large volumes secreted by ductules and ducts.
- Daily Volume: ~1000 ml.
B. Composition and Function
- Pancreatic Digestive Enzymes:
- Proteins: Trypsin, Chymotrypsin, Carboxypolypeptidase (secreted as inactive zymogens).
- Carbohydrates: Pancreatic Amylase.
- Fats: Pancreatic Lipase, Cholesterol Esterase, Phospholipase.
- Sodium Bicarbonate Solution: Neutralizes acidic chyme (creates optimal pH 7.0-8.0 for enzymes) and protects duodenal mucosa.
Activation of Pancreatic Enzymes
Secreted as zymogens to prevent self-digestion.
- Enterokinase: Enzyme on duodenal brush border. Activates Trypsinogen into Trypsin.
- Trypsin: Then activates Chymotrypsinogen and Procarboxypolypeptidase.
- Trypsin Inhibitor: Secreted by pancreas to prevent premature activation within the ducts (prevents autodigestion).
Regulation of Pancreatic Secretion
1. Acetylcholine (ACh)
From vagus/ENS. Stimulates acinar cells (enzymes).
2. Cholecystokinin (CCK)
From I-cells (response to fats/amino acids). Stimulates acinar cells (enzymes).
3. Secretin
From S-cells (response to acid). Stimulates ductal epithelium (bicarbonate solution).
Pathophysiology of the Pancreas
- Causes: Alcohol (90%), Gallstones (blocking papilla of Vater).
- Mechanism: Premature activation of enzymes leads to autodigestion.
2. Sprue (Malabsorption Syndrome): e.g., Celiac disease.
- Impaired absorption of nutrients.
- Early stage: Fat malabsorption (Steatorrhea).
- Severe: Protein/carb/vitamin malabsorption. Osteomalacia (low Ca/Vit D), Coagulation issues (low Vit K), Anemia (low B12/Folic acid).
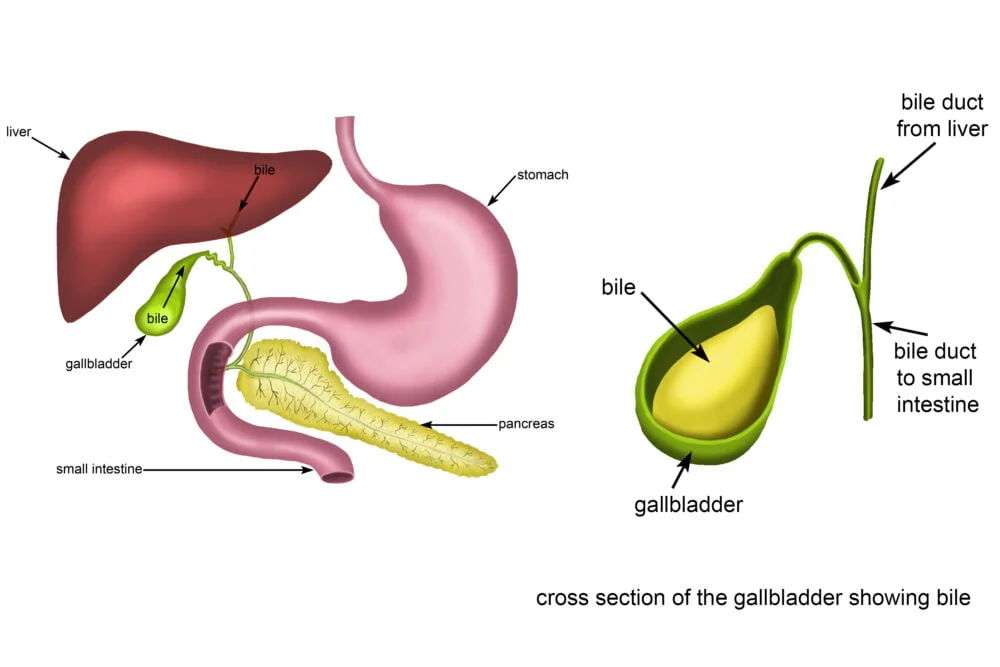
4. Bile:
Produced by hepatocytes. Daily volume: 600-1000 ml.
Functions of Bile:
- Fat Digestion/Absorption (via Bile Salts):
- Emulsification: Breaks fat globules into small droplets (increases surface area for lipase).
- Micelle Formation: Transports digested fats to the intestinal mucosa for absorption.
- Excretion of Waste: Bilirubin, excess cholesterol, toxins.
Storage: Stored and concentrated in the Gallbladder. Released when fatty chyme enters duodenum.
Regulation: CCK (most potent stimulus for contraction) and Vagal stimulation.
Effects of Reduced Biliary Secretion:
- Malabsorption of Fats (Steatorrhea).
- Deficiency of Fat-Soluble Vitamins (A, D, E, K).
- Jaundice (bilirubin accumulation).
Secretions in the Small Intestine
A. Brunner's Glands
- Location: Wall of early duodenum.
- Secretion: Alkaline Mucus.
- Function: Protects duodenal wall from acidic gastric chyme.
- Stimuli: Tactile, Vagal, Secretin. Inhibited by Sympathetic stimulation (stress -> ulcers).
B. Crypts of Lieberkühn (Intestinal Juices)
- Location: Pits between villi over entire small intestine.
- Volume: ~1800 ml/day. Rapidly reabsorbed (vehicle for absorption).
- Brush Border Enzymes: Located on enterocytes (not secreted into lumen):
- Peptidases: Split peptides into amino acids.
- Disaccharidases: Sucrase, Maltase, Isomaltase, Lactase.
- Intestinal Lipase.
Secretions of the Large Intestine
- Main Secretion: Mucus (from Crypts of Lieberkühn). Contains no enzymes.
- Regulation: Tactile stimulation, Local reflexes, Parasympathetic stimulation.
- Function: Protection from excoriation, Lubrication, Fecal binding.
Pathophysiology Related to Intestinal Function
A. Constipation
Slow movement of feces. Dry/hard feces due to excessive fluid reabsorption.
B. Megacolon (Hirschsprung's Disease)
Severe constipation. Congenital absence of ganglion cells in a segment, preventing relaxation (functional obstruction).
C. Diarrhea
Rapid movement, decreased water absorption.
- Enteritis: Inflammation (virus/bacteria).
- Psychogenic: Excessive parasympathetic stimulation (stress).
- Ulcerative Colitis: Extensive inflammation/ulceration.
GIT Secretions Quiz
Systems Physiology
Enter your details to begin the examination.
🛡️ Privacy Note: Results are for tracking and certification purposes only.
GIT Secretions Quiz
Systems Physiology
Preparing questions...
Exam Completed!
See your performance breakdown below.