Fetal Membranes, Placenta, Cord and Circulation: Safety and Feeding
The Fetal Membranes and Placenta
The fetal membranes and the placenta are temporary, yet essential, organs that develop alongside the embryo and fetus. They provide a complete life-support system, handling protection, nourishment, gas exchange, waste removal, and hormonal regulation critical for successful intrauterine development. They are expelled from the body after birth.
Formation of Embryonic Cavities and Membranes
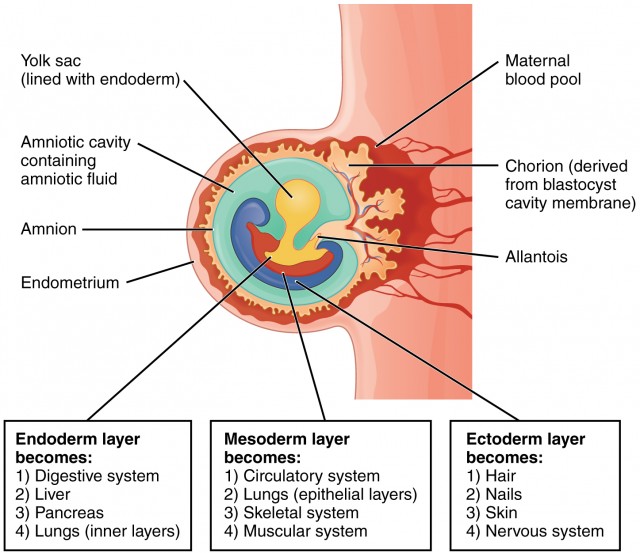
The period of early embryonic development (roughly Day 8 to Day 12-14 post-fertilization) is characterized by the rapid formation of several extraembryonic structures, which are vital for the embryo's survival and subsequent development. These include the amniotic cavity, primary and secondary yolk sacs, and the chorionic cavity, along with their associated membranes.
A. Formation of the Amniotic Cavity and Amnion
Timeline: Begins around Day 8 post-fertilization.
Process:- Cavity Formation: As the blastocyst implants, a small space appears within the epiblast, which is the dorsal layer of the bilaminar germ disc (formed from the Inner Cell Mass).
- Enlargement: This space rapidly expands to become the amniotic cavity.
- Amnioblast Differentiation: Cells from the epiblast adjacent to the cytotrophoblast differentiate into thin, flattened cells called amnioblasts.
- Amniotic Membrane Formation: These amnioblasts, along with a layer of extraembryonic mesoderm, form the amnion, which eventually encloses the entire amniotic cavity.
- Roof and Floor: The roof is formed by the amnion/cytotrophoblast, while the floor is formed by the epiblast of the bilaminar germ disc.
Key Features & Function of the Amnion/Amniotic Fluid:
-
Amniotic Sac
The amnion forms the inner lining of the amniotic sac, which will eventually surround the entire embryo and then fetus.
-
Amniotic Fluid
The cavity fills with amniotic fluid, serving crucial functions:
Protection: Acts as a shock absorber.Temp Regulation: Maintains constant temperature.Symmetry & Movement: Allows movement for musculoskeletal development.Prevents Adhesion: Stops embryo from sticking to amnion.Lung/GI Development: Fetal swallowing aids GI tract; "breathing" movements aid lungs.
B. Formation of the Yolk Sac
Timeline: Primary yolk sac begins around Day 9; Secondary yolk sac around Day 12-13.
- Cells from the hypoblast (ventral layer) migrate and line the inner surface of the cytotrophoblast.
- These cells form a thin membrane called the exocoelomic membrane (Heuser's membrane).
- This membrane + hypoblast encloses the primary yolk sac.
- Position: Bilaminar disc lies between Amniotic Cavity (dorsal) and Primary Yolk Sac (ventral).
A new layer of loose connective tissue appears and fills the space between the exocoelomic membrane/amnion externally and the cytotrophoblast internally.
- Primary sac constricts due to chorionic cavity expansion.
- A smaller, definitive secondary yolk sac forms from a portion of the primary. The larger pinched-off part degenerates.
Key Features & Function of the Yolk Sac:
Plays a role before uteroplacental circulation is functional.
Primary site of early blood cell formation (Weeks 3-6) before the liver takes over.
Precursors to sperm/eggs originate here and migrate to gonads.
In humans, it is small, regresses, and incorporates into the umbilical cord.
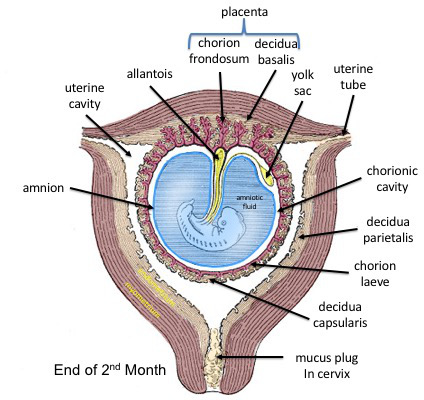
C. Formation of the Chorionic Cavity and Chorion
Timeline: Begins around Day 11-12.
Process:- Vacuole Formation: Numerous large spaces and vacuoles appear within the extraembryonic mesoderm.
- Coalescence: These fuse to form a large, isolated cavity called the chorionic cavity (extraembryonic coelom).
- Suspension of Embryo: The embryo (with amnion/yolk sac) is suspended in this cavity by the connecting stalk (future umbilical cord).
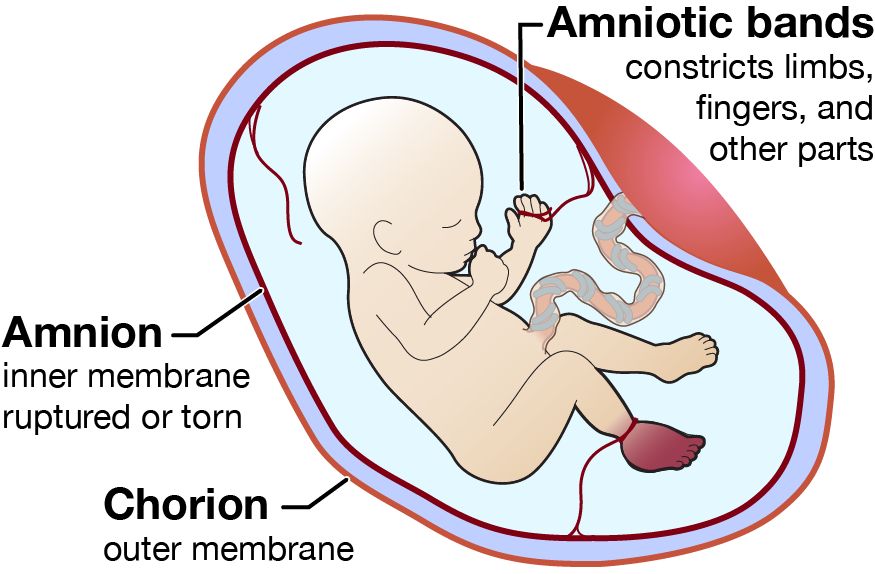
The Chorion (Outer Wall)
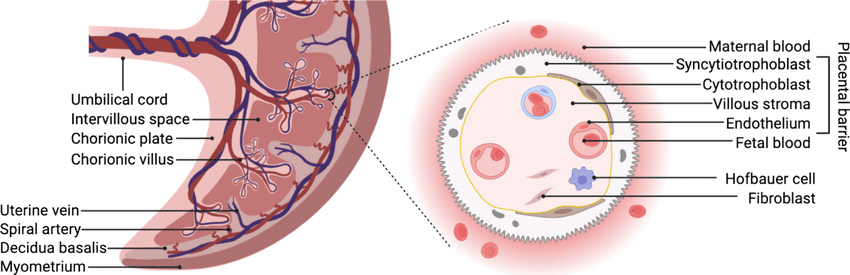
Formed by three layers:
- Syncytiotrophoblast (outermost)
- Cytotrophoblast
- Somatic layer of extraembryonic mesoderm (innermost)
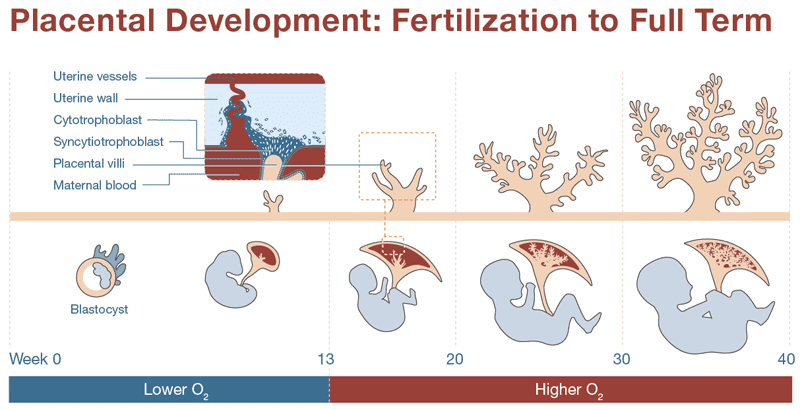
- Chorionic Villi: Gives rise to villi (functional units of placenta).
- Protection: Additional protective layer.
- Part of Placenta: The chorion frondosum forms the fetal component.
- Bilaminar germ disc centrally located.
- Dorsal: Amniotic cavity.
- Ventral: Secondary yolk sac.
- Surrounding all: Chorionic cavity (enclosed by Chorion).
- Bridge: Connecting stalk linking disc to chorion.
The Allantois: Development and Significance
Origin: Appears around Day 16-18 as a small, sausage-shaped diverticulum (outpouching) from the caudal wall of the yolk sac (hindgut) extending into the connecting stalk.
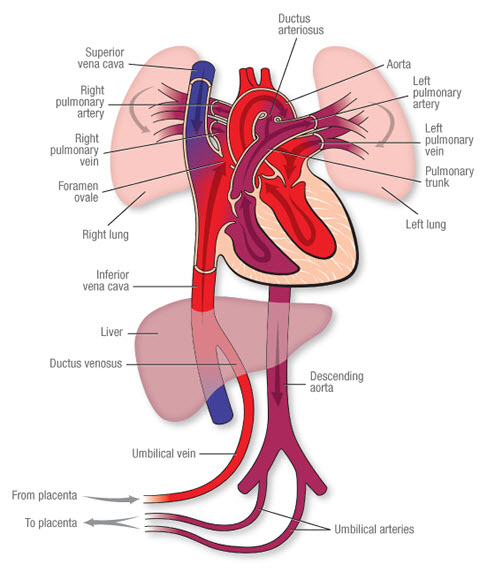
Vascular Development
The most significant role in humans. Blood vessels develop in its wall to become the umbilical arteries and umbilical vein.
These extend through the connecting stalk to link embryonic and placental circulation.
Urinary Bladder Formation
The proximal part incorporates into the developing urinary bladder.
The connection (urachus) obliterates postnatally to form the median umbilical ligament. Anomalies can lead to cysts/fistulas.
Regression & Relationship to Umbilical Cord
In humans, the allantois is largely vestigial. As the amniotic cavity expands and forms the definitive umbilical cord, the allantois regresses into a fibrous cord within it, while its vessels remain as the vital umbilical vessels.