Connective Tissue: The Body's Support System
Connective Tissue
Connective Tissue (CT) is a diverse group of tissues that connect, support, and bind other tissues and organs together. All connective tissues are derived from an embryonic tissue called mesenchyme.
Key Distinguishing Features
- Origin: All connective tissues arise from
mesenchyme. - Vascularity: Most are well vascularized, with notable exceptions being cartilage (avascular) and dense regular CT (poorly vascularized).
- Extracellular Matrix (ECM): This is the defining characteristic. Cells are widely scattered within a large amount of non-living material that they produce. The ECM, consisting of ground substance and protein fibers, is responsible for the tissue's physical properties.
Components of Connective Tissue
All connective tissues share three fundamental components: Ground Substance, Fibers, and Cells.
1. Ground Substance
An unstructured, gel-like material that fills the space between cells and contains the fibers. It is composed of:
- Interstitial Fluid: Watery fluid that bathes the cells.
- Adhesion Proteins: (e.g., fibronectin, laminin) Act as glue, allowing cells to attach to the matrix.
- Proteoglycans: Large molecules that trap water, forming a gel that allows for diffusion of nutrients and waste.
2. Fibers
Fibers provide support and strength to the connective tissue. There are three types:
Collagen Fibers
The strongest and most abundant type. Thick, rope-like bundles that provide high tensile strength (resist pulling forces).
Elastic Fibers
Long, thin, stretchy fibers containing elastin. Allow tissues to stretch and recoil. Found in skin, lungs, and blood vessels.
Reticular Fibers
Short, fine, branched collagenous fibers that form delicate networks (stroma) to support soft organs like the spleen and lymph nodes.
3. Cells of Connective Tissue
Connective tissues contain a variety of resident and migrating cells with distinct roles.
Primary Cell Types
"Blast" Cells (Immature & Active)
- Fibroblasts: In CT proper.
- Chondroblasts: In cartilage.
- Osteoblasts: In bone.
- Hematopoietic Stem Cells: In blood.
"Cyte" Cells (Mature & Maintaining)
- Fibrocytes: In CT proper.
- Chondrocytes: In cartilage.
- Osteocytes: In bone.
Other Important Cell Types:
- Adipocytes (Fat Cells): Store energy (fat), provide insulation, and cushion organs.
- Mast Cells: Initiate local inflammatory responses by releasing histamine. Found near blood vessels.
- Macrophages: "Big eaters" that engulf foreign materials and dead cells as part of the immune system.
- Plasma Cells: Produce antibodies.
- Leukocytes (White Blood Cells): Migrate from the bloodstream to fight infection.
Primary Functions & Main Categories
The diverse composition of connective tissues allows them to perform a wide range of functions, from binding and support to transportation and immune response. They are broadly classified into four main categories.
1. Connective Tissue Proper
Includes Loose CT (e.g., Areolar, Adipose) and Dense CT (e.g., tendons, dermis of the skin).
2. Cartilage
Strong and flexible tissue that provides support and shock absorption. Includes Hyaline, Elastic, and Fibrocartilage.
3. Bone Tissue
Hard connective tissue that forms the skeleton, with a calcified matrix.
4. Blood
A fluid connective tissue where the extracellular matrix is the liquid plasma.
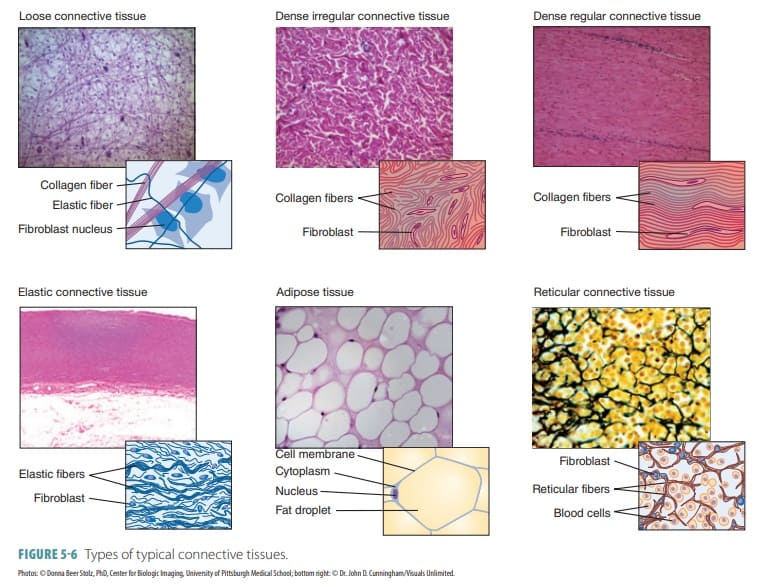
Connective Tissue Proper
This is the most diverse group of connective tissues. It is divided into two main categories: Loose Connective Tissues, which have more ground substance and fewer fibers, and Dense Connective Tissues, which have more fibers and less ground substance.
A. Loose (Areolar) Connective Tissues
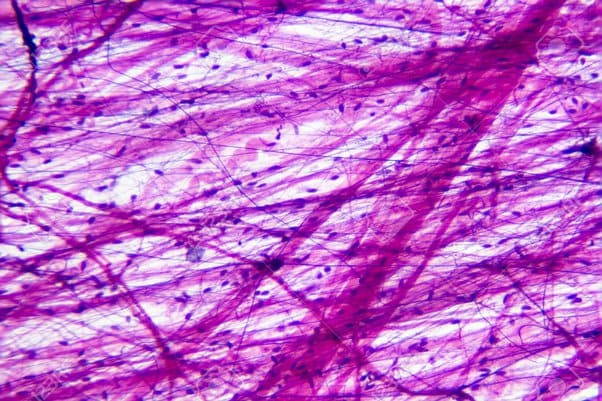
Loose Areolar Connective Tissue
Features a loose, gel-like matrix with all three fiber types (collagen, elastic, reticular) and various cells, including fibroblasts, macrophages, and mast cells.
Histology Hint:
Look for a sparse, web-like appearance with randomly arranged thick pink (collagen) and thin black/purple (elastic) fibers, plus many scattered black dots (cell nuclei).

Adipose Tissue (Fat)
Primarily composed of large, tightly packed adipocytes (fat cells) with very little matrix. It is highly vascularized.
Histology Hint:
Characterized by large, empty-looking circular cells (adipocytes), as the fat droplet is typically dissolved during processing. Nuclei are flattened and pushed to the periphery.
Reticular Connective Tissue
A network of fine reticular fibers in a loose ground substance, with reticular cells (specialized fibroblasts) as the main cell type.
Histology Hint:
Look for a fine, branching network of dark-staining reticular fibers forming a delicate meshwork (stroma), typically filled with numerous small, round cells (like lymphocytes in a lymph node).
B. Dense (Fibrous) Connective Tissues
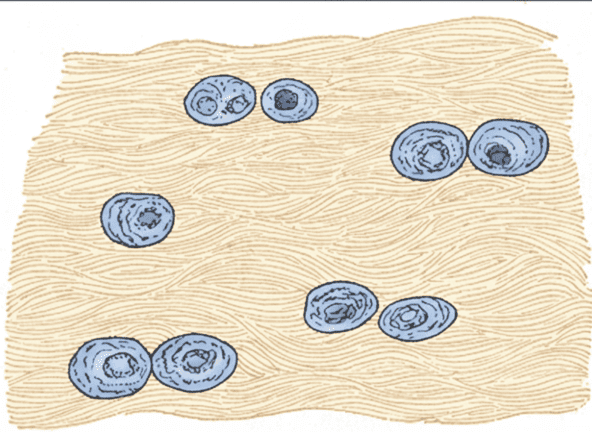
Dense Regular Connective Tissue
Densely packed, primarily parallel collagen fibers with fibroblasts as the major cell type. It is poorly vascularized.
Histology Hint:
Characterized by dense, wavy, parallel bundles of pink collagen fibers running in a single direction, with fibroblast nuclei squeezed and flattened between them.
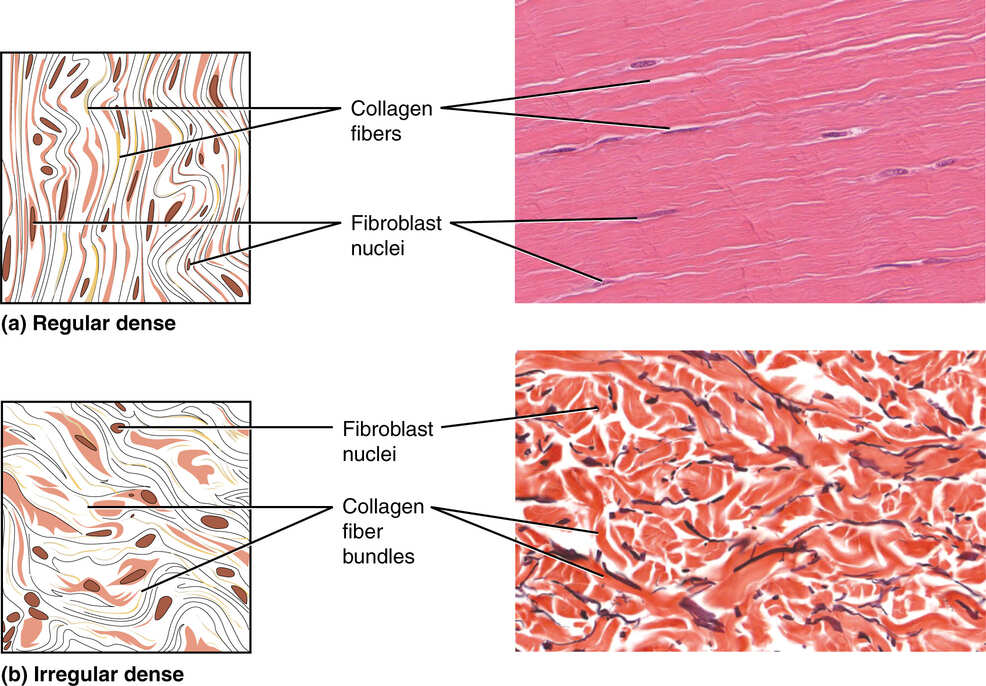
Dense Irregular Connective Tissue
Primarily irregularly arranged, thick collagen fibers with some elastic fibers and fibroblasts.
Histology Hint:
Shows thick bundles of pink collagen fibers running in many different directions, creating a chaotic appearance.
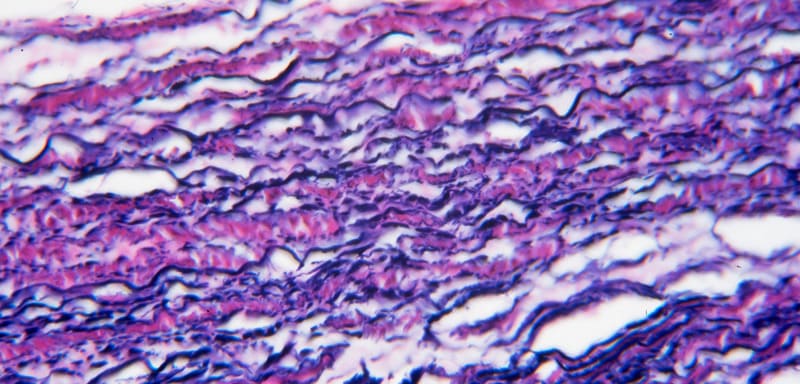
Elastic Connective Tissue
A type of dense regular connective tissue with a high proportion of elastic fibers.
Histology Hint:
Displays prominent, wavy, dark-staining elastic fibers arranged in parallel, often with a background of lighter pink collagen.

Cartilage
Cartilage is a tough, flexible connective tissue that consists of a firm, gelatinous matrix in which cartilage cells, or chondrocytes, are embedded within fluid-filled spaces called lacunae. It is avascular (lacks blood vessels) and lacks nerves, relying on diffusion for nutrients.
Key Characteristics:
- Cells: Chondroblasts produce the matrix, which mature into chondrocytes that maintain it from within their lacunae.
- Matrix: A firm, gel-like ground substance rich in water, proteoglycans, and fibers.
- Perichondrium: Most cartilages are surrounded by a dense irregular connective tissue membrane that provides nutrients.
Types of Cartilage
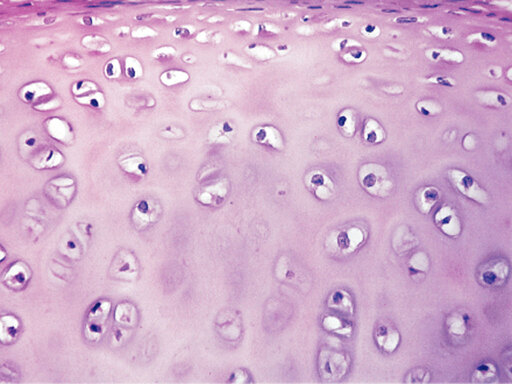
1. Hyaline Cartilage
The most abundant type, with a smooth, glassy, bluish-white appearance. It provides a protective covering on bone surfaces, forms the larynx, connects ribs to the sternum, and supports air passages.
Histology Details:
What is in between the lacunae? A firm, glassy matrix of water, proteoglycans, and very fine collagen fibers (not usually visible).
How far apart are the lacunae? Moderately spaced, allowing for an even distribution of chondrocytes.
Function: Supports and reinforces, provides resilient cushioning, and resists compressive stress.
Location: Articular cartilages of joints, costal cartilages of ribs, cartilages of the nose, trachea, and larynx.
2. Elastic Cartilage
Similar to hyaline cartilage, but contains an abundance of visible elastic fibers that provide greater elasticity and flexibility.
Histology Details:
What is in between the lacunae? A matrix containing visible, dark-staining elastic fibers in addition to collagen and proteoglycans.
How far apart are the lacunae? Moderately spaced, similar to hyaline, but the elastic fibers give it a more flexible appearance.
Function: Maintains the shape of a structure while allowing great flexibility.
Location: External ear (pinna), epiglottis.
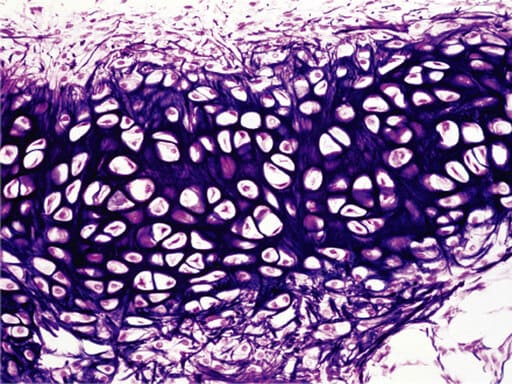
3. Fibrocartilage
The matrix contains many tightly packed, thick collagen fibers that lie between short rows of chondrocytes. It is especially tough and able to absorb significant shocks and pressure.
Histology Details:
What is in between the lacunae? A matrix dominated by thick, often parallel bundles of collagen fibers, with less ground substance.
How far apart are the lacunae? Chondrocytes are often arranged in rows between the thick fiber bundles, making them more sparsely distributed than in other cartilage types.
Function: High tensile strength with the ability to absorb compressive shock.
Location: Intervertebral discs, pubic symphysis, menisci of the knee joint.

Bone (Osseous Tissue)
Of all the supportive connective tissues, bone is the hardest and most rigid. This results from its unique matrix, which is composed of inorganic calcium salts (for hardness) and organic collagen fibers (for flexibility). It is well vascularized and contains specialized cells: osteoblasts (which form the matrix) and osteocytes (which maintain it from within lacunae).
Compact Bone (The "Hard Outer Shell")
This is the dense, solid outer layer of almost all bones, built for strength and protection. It is organized into repeating, cylindrical units called osteons (Haversian systems).

Spongy Bone (The "Porous Inner Core")
This is the lighter, porous inner layer of most bones, made of a network of needle-like pieces called trabeculae. The spaces between trabeculae are filled with red bone marrow, where blood cells are produced.
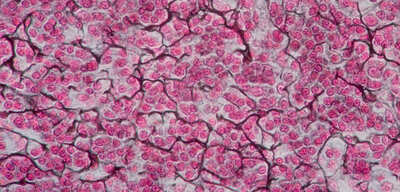
Blood
Blood is the only fluid connective tissue. It consists of blood cells (formed elements) suspended in a fluid matrix called plasma.
Primary Functions:
- Transportation: Delivers oxygen, nutrients, and hormones; carries away waste products.
- Regulation: Helps maintain body temperature, pH, and fluid volume.
- Protection: Prevents blood loss through clotting and prevents infection with antibodies and white blood cells.
1. Plasma (The Extracellular Matrix)
The non-living, straw-colored fluid matrix that makes up about 55% of total blood volume. It is ~90% water and contains numerous solutes.
Key Solutes:
- Plasma Proteins: Albumins (maintain osmotic pressure), Globulins (antibodies, transport), Fibrinogen (clotting).
- Other Solutes: Nutrients, electrolytes, respiratory gases, hormones, and waste products.
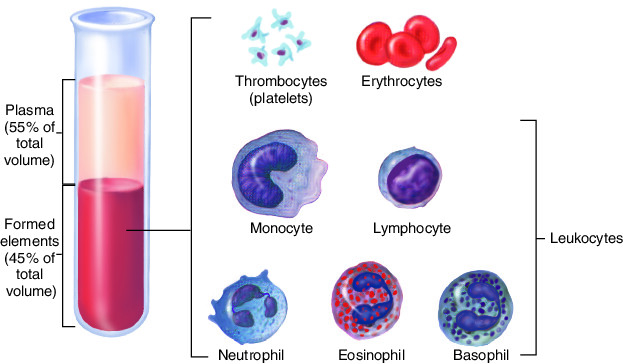
2. Formed Elements (The Cells)
The living cellular components suspended in plasma, making up about 45% of total blood volume. All are formed in the bone marrow.
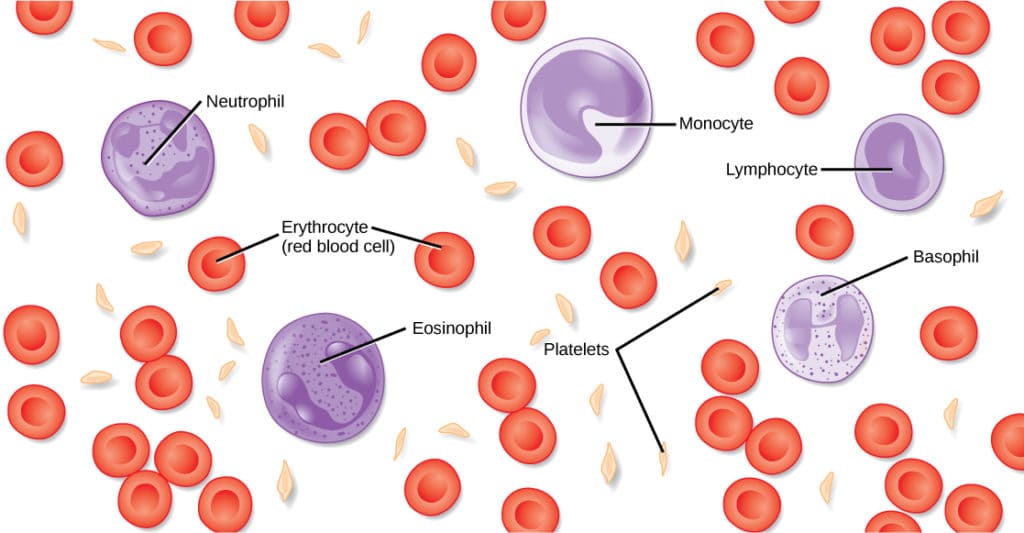
a. Erythrocytes (Red Blood Cells - RBCs)
Anucleated, biconcave discs filled with hemoglobin. Their primary function is oxygen transport.
b. Leukocytes (White Blood Cells - WBCs)
Complete cells crucial for immunity and defense. Includes Neutrophils, Lymphocytes, Monocytes, Eosinophils, and Basophils.
c. Thrombocytes (Platelets)
Cytoplasmic fragments, not true cells. Essential for blood clotting (hemostasis).
Test Your Knowledge
Check your understanding of the concepts covered in this post.
1. Which of the following is a primary characteristic of all connective tissues?
- Cells are tightly packed with little extracellular material.
- It is always avascular.
- It contains a significant amount of extracellular matrix.
- Its primary function is protection from abrasion.
2. The major components of the extracellular matrix in connective tissue are:
- Cells and ground substance.
- Ground substance and protein fibers.
- Protein fibers and specialized cells.
- Blood vessels and nerve endings.
3. Which cell type is primarily responsible for producing the fibers and ground substance in most connective tissues?
- Macrophages
- Adipocytes
- Fibroblasts
- Chondrocytes
4. All of the following are types of protein fibers found in connective tissue EXCEPT:
- Collagen fibers
- Elastic fibers
- Reticular fibers
- Myosin fibers
5. Which type of fiber provides great tensile strength, allowing tissue to resist stretching and pulling, and is the most abundant protein in the body?
- Elastic fibers
- Collagen fibers
- Reticular fibers
- Actin fibers
6. The "ground substance" of connective tissue primarily consists of:
- Water, ions, and lipids.
- Interstitial fluid, cell adhesion proteins, and proteoglycans.
- Collagen and elastic fibers.
- Blood plasma and platelets.
7. Which type of connective tissue cell is responsible for storing fat and providing insulation?
- Mast cells
- Macrophages
- Adipocytes
- Lymphocytes
8. A rich blood supply, or vascularity, is a general feature of most connective tissues, with the notable exception of:
- Areolar connective tissue
- Dense regular connective tissue
- Adipose tissue
- Cartilage
9. What is the primary function of mast cells in connective tissue?
- Phagocytosis of foreign invaders.
- Production of antibodies.
- Initiation of the inflammatory response.
- Storage of energy reserves.
10. Which statement best describes the general organization of connective tissue?
- Cells are closely opposed and form continuous sheets.
- It always forms the lining of cavities and surfaces.
- Cells are often widely scattered within an abundant extracellular matrix.
- It is primarily composed of contractile proteins.
11. The protein fiber that allows for stretch and recoil in connective tissue is the ___________ fiber.
12. The jelly-like or fluid material that fills the space between cells and fibers in connective tissue is called the _____________.
13. The most common fixed cell type in general connective tissue proper is the _____________, which synthesizes fibers and ground substance.
14. _______________ are large, irregular cells in connective tissue that are specialized for phagocytosis to engulf foreign particles and cellular debris.
15. Unlike epithelial tissue, connective tissue is typically rich in _____________, allowing for efficient nutrient and waste exchange.
Quiz Complete!
Your Score:
0%
0 / 0 correct