Cardiovascular System Anatomy: For the love of the Heart
Introduction to the Cardiovascular System
The cardiovascular system, also known as the circulatory system, is a vast network responsible for transporting blood throughout the entire body. This system is essential for maintaining life and ensuring that every cell receives what it needs to function properly.
Key Components
The cardiovascular system is primarily composed of three main parts, working in perfect concert.
The Heart
This muscular organ, roughly the size of a clenched fist, is the central pump of the system. It continuously contracts and relaxes, driving blood through the vast network of vessels.
Blood Vessels
Arteries:
Carry oxygenated blood away from the heart. Their thick, muscular walls withstand high pressure.
Veins:
Carry deoxygenated blood back to the heart. Their thinner walls and internal valves prevent backward blood flow.
Capillaries:
The smallest vessels, forming vast networks that connect arteries and veins. Their ultra-thin walls allow for the efficient exchange of gases, nutrients, and waste products with the body's cells.
Blood
Plasma:
The liquid matrix, mostly water, that carries dissolved nutrients, hormones, and waste.
Red Blood Cells (Erythrocytes):
Contain hemoglobin to transport oxygen from the lungs to tissues and return carbon dioxide.
White Blood Cells (Leukocytes):
Key components of the immune system, defending the body against pathogens.
Platelets (Thrombocytes):
Small cell fragments essential for initiating the blood clotting process to stop bleeding.
Primary Functions
The cardiovascular system performs several indispensable functions to maintain homeostasis and sustain life.
Transport of O₂ & Nutrients
Delivers oxygen and nutrients to every cell for energy and metabolic processes.
Removal of Waste
Collects metabolic waste like CO₂ and urea and transports them to the lungs and kidneys for excretion.
Hormone Transport
Acts as a delivery system for hormones, carrying them from glands to their target organs.
Temperature Regulation
Distributes heat throughout the body and regulates its dissipation to maintain a stable internal temperature.
Protection Against Disease
Circulates white blood cells and antibodies as part of the immune system to fight infections.
Blood Clotting
Platelets and clotting factors in the blood prevent excessive blood loss at sites of injury.
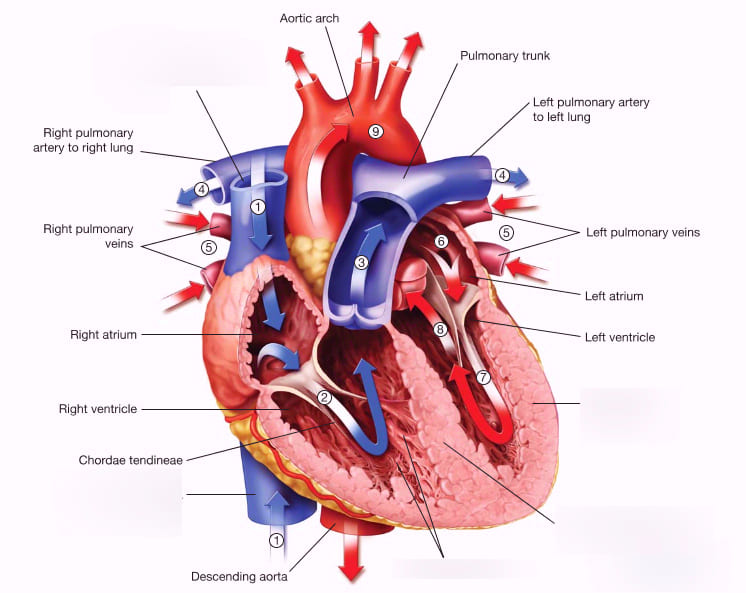
Anatomy of the Heart and Great Vessels
The heart is a hollow, muscular organ located in the mediastinum, the central compartment of the thoracic cavity, nestled between the lungs. It sits slightly to the left of the midline, resting on the diaphragm. Its pointed end, the apex, points inferiorly and to the left, while the broader base points superiorly and to the right.
I. The Pericardium: The Heart's Protective Sac
The heart is encased in a double-walled sac called the pericardium. It serves to anchor the heart, prevent it from overfilling, and provide a frictionless environment for its constant beating.
Fibrous Pericardium
The tough, outermost layer made of dense connective tissue. It anchors the heart to the diaphragm and great vessels, preventing overfilling and providing a strong protective barrier.
Serous Pericardium
A thinner, delicate inner layer, itself composed of two sub-layers:
- Parietal Layer: Lines the inside of the fibrous pericardium.
- Visceral Layer (or Epicardium): Adheres directly to the surface of the heart muscle.
- Pericardial Cavity: The potential space between the parietal and visceral layers, containing a thin film of serous fluid that acts as a lubricant to eliminate friction during heartbeats.
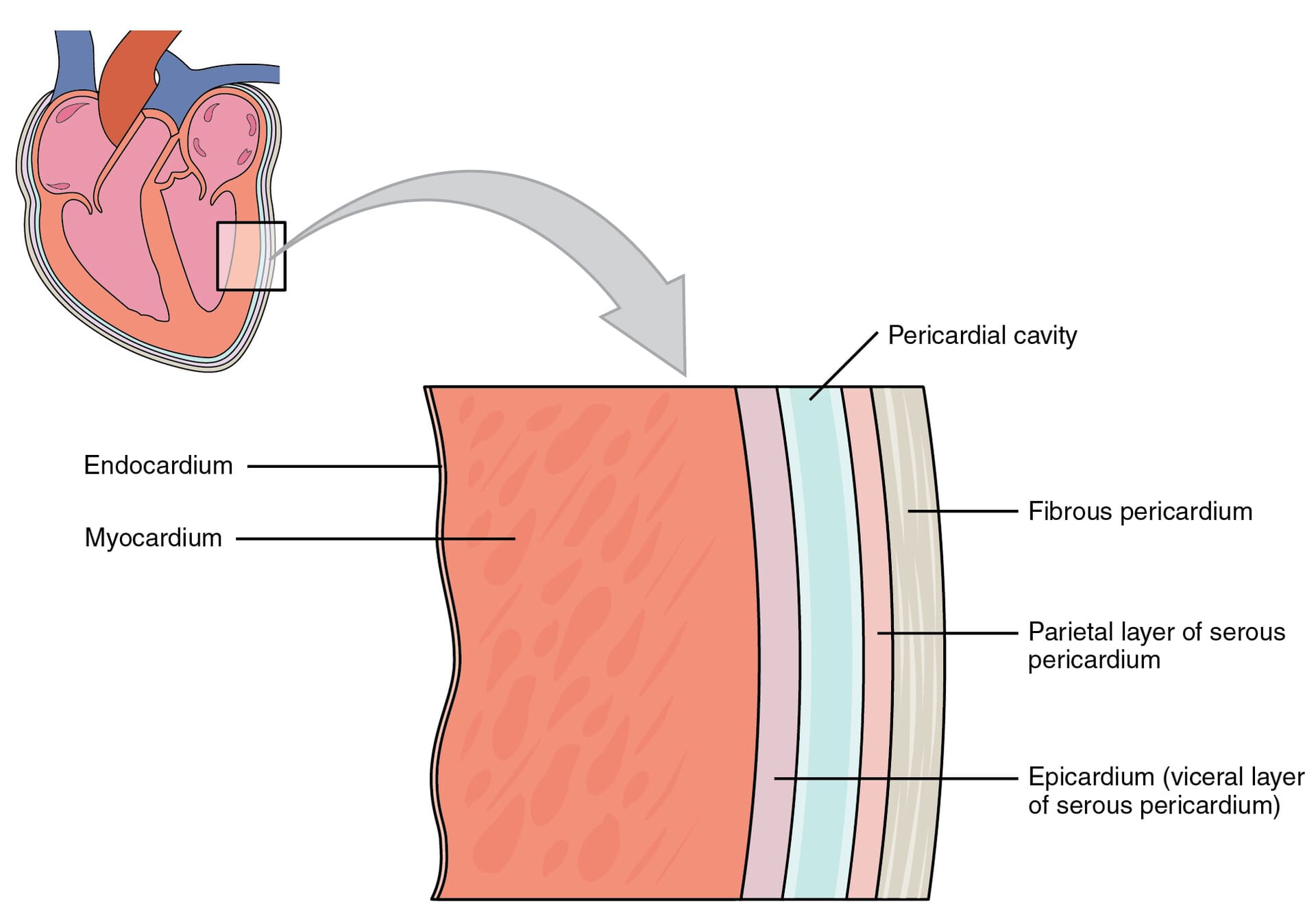
II. Layers of the Heart Wall
The wall of the heart itself is composed of three distinct layers, from superficial to deep.
1. Epicardium
The outermost layer (and also the visceral layer of the serous pericardium). It is a protective layer that contains the coronary blood vessels and adipose tissue.
2. Myocardium
The thick, muscular middle layer composed of cardiac muscle cells (cardiomyocytes). This is the contractile layer responsible for the heart's pumping action. Its thickness is greatest in the left ventricle.
3. Endocardium
The innermost layer, a thin, smooth membrane that lines the heart's chambers and covers the valves. Its smooth surface minimizes friction and prevents clot formation.
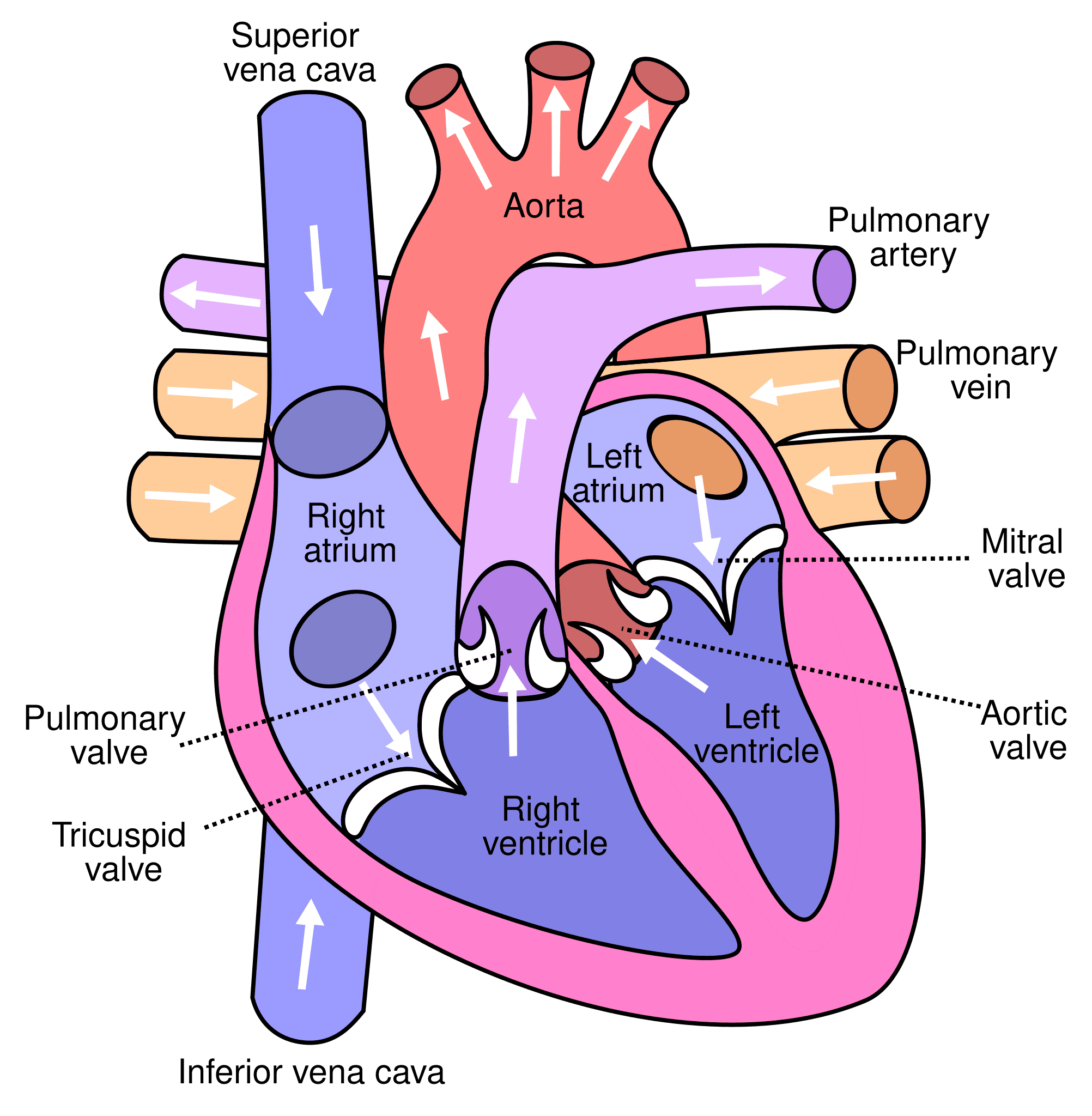
III. Chambers of the Heart
The heart is a four-chambered organ, divided by a muscular septum into right and left sides. This separation is crucial for ensuring that oxygen-poor and oxygen-rich blood do not mix.
Right Atrium (RA)
- Receives deoxygenated blood from the body via the Superior Vena Cava (SVC), Inferior Vena Cava (IVC), and Coronary Sinus.
- Pumps blood to the right ventricle.
Left Atrium (LA)
- Receives oxygenated blood from the lungs via the four pulmonary veins.
- Pumps blood to the left ventricle.
Right Ventricle (RV)
- Receives deoxygenated blood from the right atrium.
- Pumps deoxygenated blood to the lungs via the pulmonary artery.
Left Ventricle (LV)
- Receives oxygenated blood from the left atrium.
- The strongest chamber; pumps oxygenated blood to the entire body via the aorta.
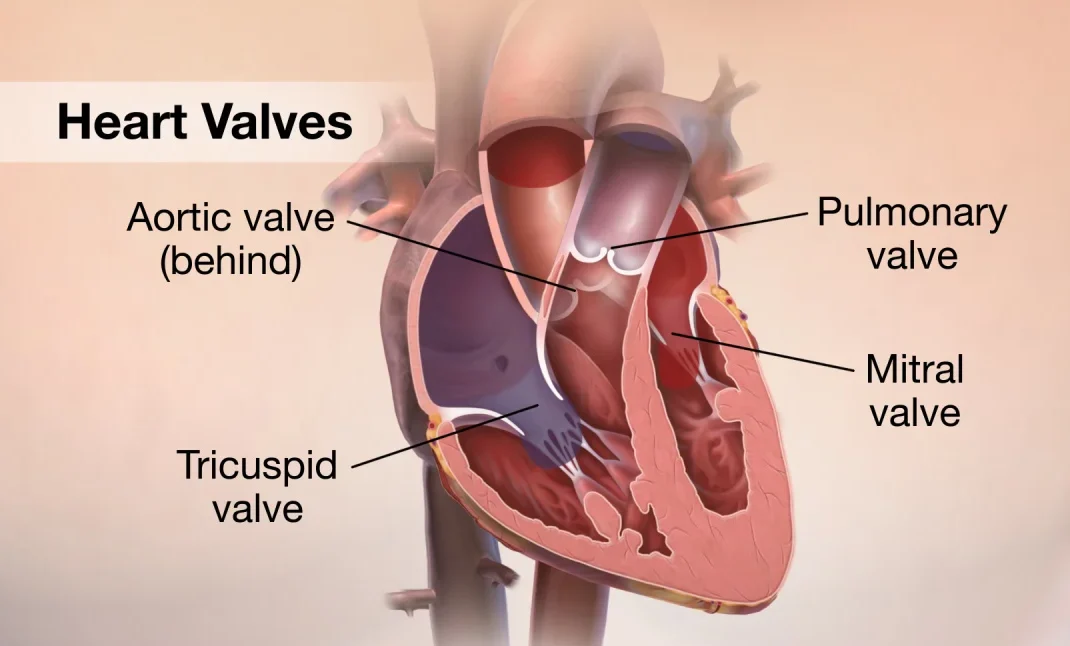
IV. Heart Valves: Ensuring Unidirectional Blood Flow
The heart contains four valves that act as one-way doors, preventing the backflow of blood (regurgitation). They open and close passively in response to pressure changes within the chambers.
Atrioventricular (AV) Valves
Located between the atria and ventricles.
- Tricuspid Valve: Between the right atrium and right ventricle (has three cusps).
- Mitral (Bicuspid) Valve: Between the left atrium and left ventricle (has two cusps).
The AV valves are anchored by fibrous chordae tendineae ("heart strings") to papillary muscles in the ventricles. When the ventricles contract, these muscles pull on the cords, preventing the valve flaps from being pushed back up into the atria.
Semilunar (SL) Valves
Located at the exit of the ventricles, preventing blood from flowing back from the great arteries.
- Pulmonary Valve: Between the right ventricle and the pulmonary artery.
- Aortic Valve: Between the left ventricle and the aorta.
V. Great Vessels of the Heart
These are the major blood vessels that are directly connected to the heart, responsible for carrying blood to and from its chambers.
Note: It's an artery because it carries blood AWAY from the heart.
Note: They are veins because they carry blood TOWARDS the heart.
Formation and Structure of the Heart (Embryonic Development)
The development of the heart is an intricate process that begins very early in embryonic life, transforming a simple tube into a four-chambered pump. This process is critical, as even minor errors can lead to significant congenital heart defects.
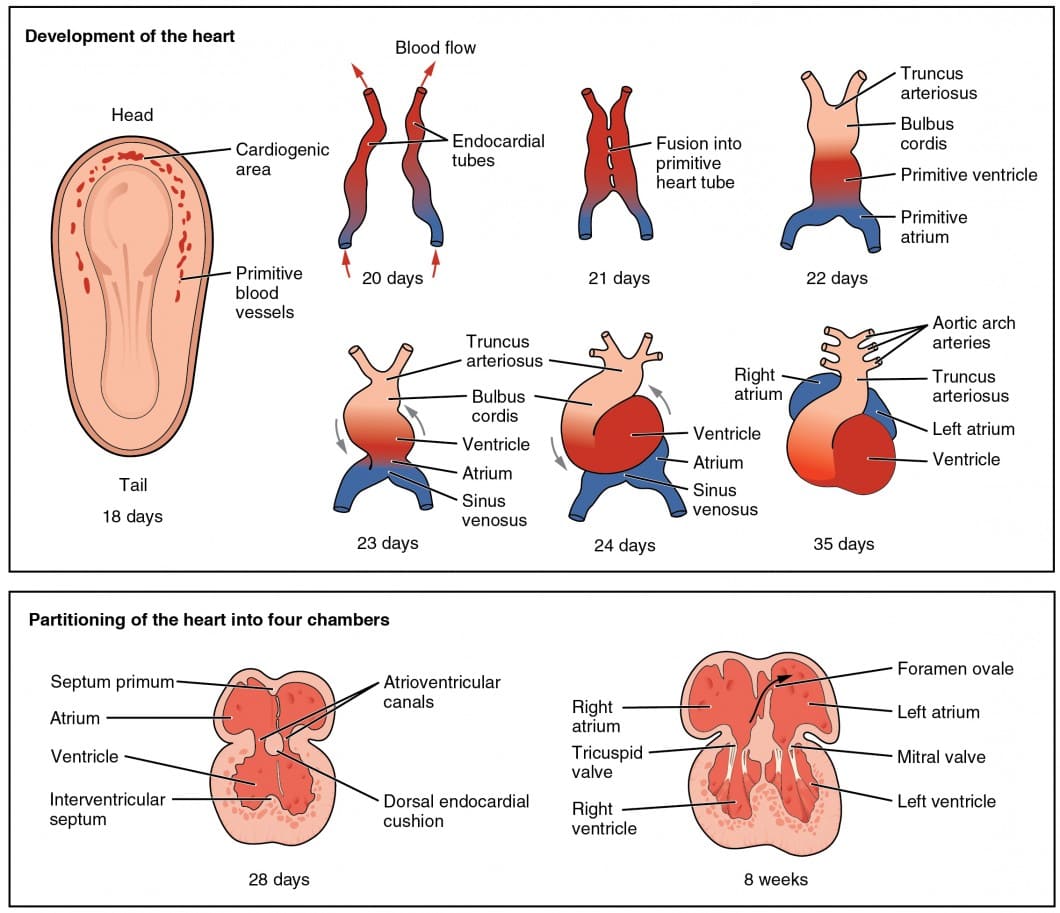
I. Early Origins: The Cardiogenic Field and Tube Formation
Around day 18-19, specialized mesenchymal cells in the cardiogenic field (a horseshoe-shaped area in the cranial end of the embryo) begin to form two separate endocardial tubes.
II. Fusion of the Endocardial Tubes and Positional Changes
As the embryo undergoes lateral and cephalic (head) folding, the two endocardial tubes are brought to the midline and, by day 21-22, fuse to form a single, straight primitive heart tube.
III. Elongation and Cardiac Looping
Beginning around day 23, the rapidly elongating heart tube, fixed at both ends, begins to bend and fold upon itself. This crucial process, known as cardiac looping, establishes the basic left-right asymmetry and positions the future chambers into their correct anatomical relationships.
IV. Formation of Septa and Chambers (Septation)
Occurring roughly between weeks 4 and 5, the single tube undergoes a complex series of septation events to create the four-chambered heart.
1. Atrial Septation
The primitive atrium is divided into right and left atria by the growth of the septum primum and septum secundum, leaving a critical fetal opening called the foramen ovale.
2. Ventricular Septation
The primitive ventricle is divided into right and left ventricles by the growth of the muscular and membranous parts of the interventricular septum.
3. Atrioventricular (AV) Septation
The common AV canal is divided into right and left openings by the fusion of endocardial cushions, which are also crucial for valve formation.
4. Outflow Tract Septation
A spiral aorticopulmonary septum grows and divides the single outflow tract (truncus arteriosus) into the aorta and the pulmonary artery, establishing their correct anatomical relationship.
V. Valve Formation
The four heart valves (tricuspid, mitral, aortic, pulmonary) develop from specialized mesenchymal tissue (endocardial cushions and tubercles) around the AV canals and outflow tracts. This tissue is remodeled and hollowed out by blood flow to form the functional cusps and leaflets.
VI. Vascular Development: Building the Circulatory Network
Occurring concurrently with heart development, the formation of the body's vast network of blood vessels is essential for embryonic survival and growth.
Vasculogenesis
The de novo (new) formation of blood vessels from endothelial progenitor cells (angioblasts), which coalesce into a primary vascular network.
Angiogenesis
The formation of new blood vessels by sprouting or splitting from pre-existing ones. This process expands and remodels the initial network.
This entire process is tightly regulated by a sophisticated interplay of growth factors like VEGF and signaling pathways like Notch, ensuring vessels mature, stabilize, and acquire their distinct arterial or venous identities.
Congenital Heart Diseases (CHD)
Congenital Heart Disease refers to cardiac anomalies present at birth, arising from defects in the heart's structure or function, including the great vessels. These lesions can either obstruct blood flow or alter the normal pathway of blood circulating through the heart.
Etiological Factors
The development of CHD can be influenced by a combination of environmental and genetic factors.
Environmental Factors
- Viral Infections: Rubella during the first trimester.
- Medications: Lithium, Accutane, some anti-seizure drugs.
- Substances: Alcohol (FAS), smoking, cocaine.
- Maternal Illnesses: Diabetes, PKU, folic acid deficiency.
Genetic Factors
- Heredity: Family history of heart defects.
- Gene Mutations: Can disrupt normal heart development.
- Associated Syndromes: High incidence with Down syndrome and Turner syndrome.
Classification of CHD
Acyanotic Heart Defects ("Pink Babies")
In these defects, blood flow is altered, but there is no significant decrease in blood oxygen saturation, so cyanosis (bluish skin) is not present at birth. They are divided into two main groups:
A. Left-to-Right Shunts
- Atrial Septal Defect (ASD)
- Ventricular Septal Defect (VSD)
- Patent Ductus Arteriosus (PDA)
- AV Canal Defect
B. Obstructive Lesions
- Coarctation of the Aorta
- Aortic Stenosis
- Pulmonic Stenosis
Common Acyanotic Defects Explained
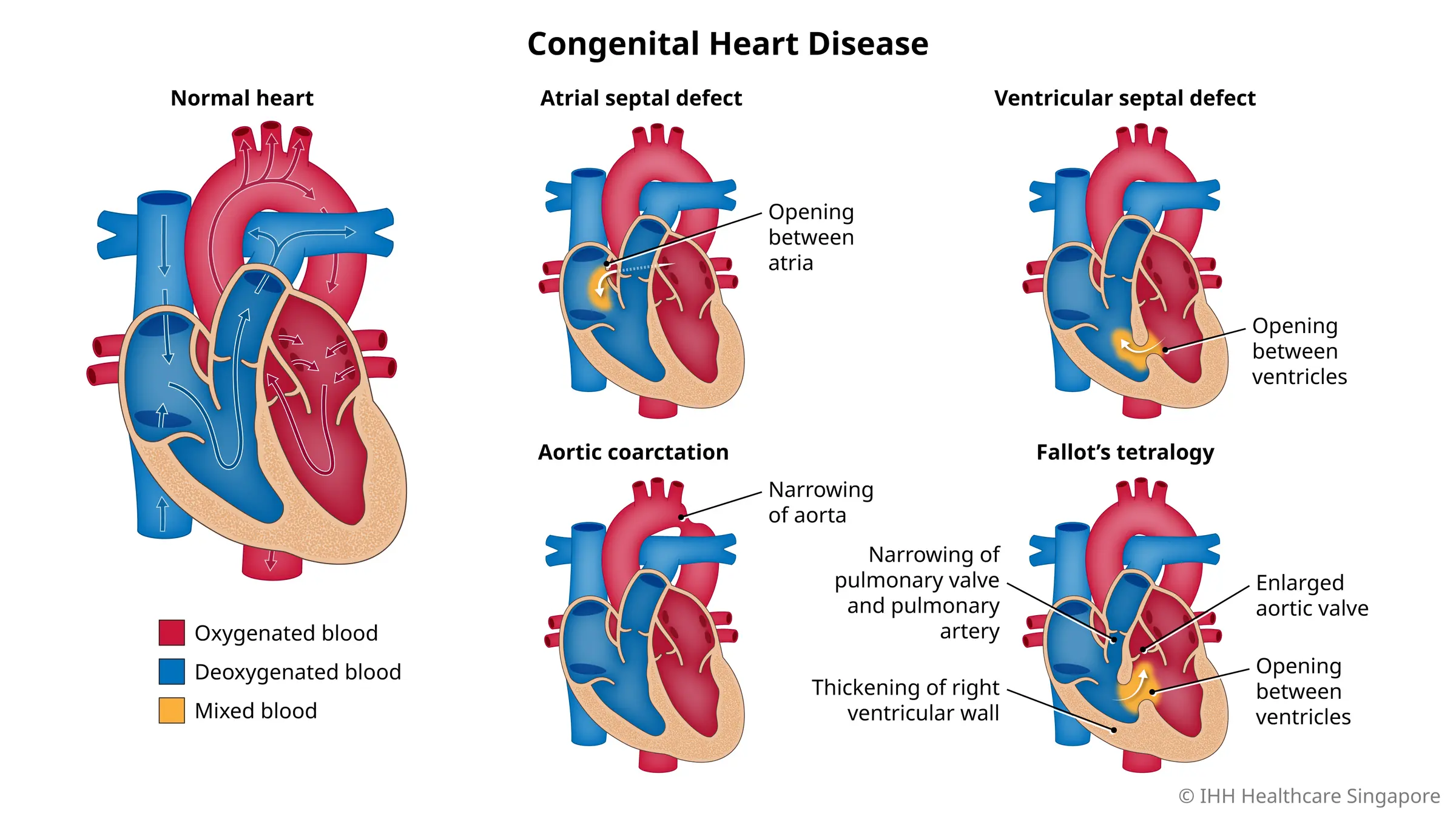
1. Atrial Septal Defect (ASD)
A hole in the wall (septum) separating the heart's two upper chambers (atria). This allows oxygen-rich blood to leak from the left atrium into the right atrium, leading to increased blood flow to the lungs. Small ASDs may close on their own, while larger ones might require intervention to prevent complications like pulmonary hypertension or heart failure.
2. Ventricular Septal Defect (VSD)
A hole in the wall (septum) separating the heart's two lower chambers (ventricles). This allows oxygen-rich blood to flow from the left ventricle into the right ventricle, causing the right side of the heart to work harder and increasing blood flow to the lungs. VSDs are among the most common congenital heart defects and can range from small, asymptomatic holes to large defects requiring surgical repair.
3. Patent Ductus Arteriosus (PDA)
The ductus arteriosus is a blood vessel connecting the aorta and pulmonary artery that is essential for fetal circulation. Normally, it closes shortly after birth. In PDA, this vessel remains open, allowing oxygen-rich blood from the aorta to flow back into the pulmonary artery and overload the lungs. This can lead to increased work for the heart and potential lung problems if not treated.
4. AV Canal Defect (Atrioventricular Septal Defect)
This is a complex heart defect involving a large hole in the center of the heart where the upper and lower chambers meet, often with a single, common valve instead of separate mitral and tricuspid valves. This allows oxygen-rich and oxygen-poor blood to mix and causes increased blood flow to the lungs. It is commonly associated with Down syndrome and usually requires surgical correction.
5. Coarctation of the Aorta (CoA)
A narrowing of the aorta, the body's main artery that carries oxygen-rich blood from the heart to the rest of the body. This narrowing typically occurs just beyond the arteries branching off to the upper body. The coarctation obstructs blood flow to the lower body, leading to high blood pressure in the upper body and head, and lower blood pressure in the legs and abdomen.
6. Pulmonary Stenosis (PS)
A narrowing of the pulmonary valve, the valve that controls blood flow from the heart's right ventricle to the pulmonary artery and then to the lungs. This narrowing makes the heart work harder to pump blood to the lungs, which can lead to thickening of the right ventricle wall and, in severe cases, right-sided heart failure.
7. Aortic Stenosis (AS)
A narrowing of the aortic valve, the valve that controls blood flow from the heart's left ventricle to the aorta and then to the rest of the body. This narrowing forces the left ventricle to pump harder to push blood through the constricted valve, leading to thickening of the left ventricle wall and potentially reducing the heart's ability to pump blood effectively.
Cyanotic Heart Defects ("Blue Babies")
These defects result in a mixing of oxygenated and deoxygenated blood within the heart or great vessels, leading to decreased blood oxygen saturation and a characteristic bluish discoloration of the skin and mucous membranes (cyanosis).
Decreased Pulmonary Blood Flow
- Tetralogy of Fallot
- Tricuspid Atresia
- Pulmonary Atresia with VSD
Mixed Blood Flow
- Transposition of the Great Arteries
- Total Anomalous Pulmonary Venous Return
- Truncus Arteriosus
- Hypoplastic Left Heart Syndrome
Cyanotic Heart Defects - The "5 T's" Trick!
The 5 main cyanotic congenital heart defects are easy to remember because they all start with the letter "T".
- Truncus Arteriosus
- Transposition
- Tricuspid Atresia
- Tetralogy of Fallot
- TAPVR
The 5 Main "T" Defects Explained
Truncus Arteriosus
Instead of two separate arteries leaving the heart, there is only one large artery (the truncus) that then divides to supply blood to both the lungs and the body. A VSD is almost always present.
Transposition of the Great Arteries
The aorta and pulmonary artery are switched. The aorta arises from the right ventricle and the pulmonary artery from the left, creating two separate, parallel circuits. A connection (PDA, ASD, or VSD) is essential for survival at birth.
Tricuspid Atresia
The tricuspid valve is missing, meaning blood cannot flow from the right atrium to the right ventricle. Survival depends on an ASD and VSD to allow blood to reach the lungs.
Tetralogy of Fallot
A combination of four defects: a large VSD, pulmonary stenosis (narrowing), an overriding aorta, and right ventricular hypertrophy. The stenosis restricts blood flow to the lungs, forcing deoxygenated blood through the VSD into the aorta.
Total Anomalous Pulmonary Venous Return (TAPVR)
The four pulmonary veins, which should carry oxygenated blood to the left atrium, instead connect abnormally to the right atrium or another systemic vein. This causes all oxygenated and deoxygenated blood to mix in the right heart.
Cyanotic Heart Defects - Recap!
Remember the 5 T's and count them on your fingers:
- 1 finger:Truncus Arteriosus - 1 great vessel leaves the heart instead of 2.
- 2 fingers (crossed):Transposition - The 2 great arteries are reversed.
- 3 fingers:Tricuspid Atresia - The tricuspid valve (3 leaflets) fails to form.
- 4 fingers:Tetralogy of Fallot - A tetrad of 4 cardiac defects.
- 5 fingers:Total Anomalous Pulmonary Venous Return - 5 words in the name.
Test Your Knowledge
Check your understanding of the Respiratory System's development and function.
1. Which of the following is the primary function of the respiratory system?
- Digestion of nutrients
- Regulation of body temperature
- Gas exchange (oxygen and carbon dioxide)
- Blood filtration
2. During fetal development, the respiratory system originates from which germ layer?
- Ectoderm
- Mesoderm
- Endoderm
- Neuroectoderm
3. The production of surfactant, crucial for preventing alveolar collapse, begins to significantly increase during which stage of lung maturation?
- Pseudoglandular stage
- Canalicular stage
- Saccular stage
- Alveolar stage
4. Respiratory Distress Syndrome (RDS) in newborns is primarily caused by:
- Bacterial infection
- Incomplete development of the diaphragm
- Insufficient production of pulmonary surfactant
- Structural abnormalities of the trachea
5. Which of the following describes the condition where the trachea fails to properly separate from the esophagus during development?
- Bronchial atresia
- Tracheoesophageal fistula
- Congenital diaphragmatic hernia
- Pulmonary hypoplasia
6. Which part of the respiratory system is responsible for warming, humidifying, and filtering inhaled air?
- Alveoli
- Bronchioles
- Upper respiratory tract (nasal cavity, pharynx, larynx)
- Diaphragm
7. A congenital diaphragmatic hernia (CDH) is characterized by:
- An abnormal opening in the chest wall.
- A portion of the diaphragm being underdeveloped, allowing abdominal contents to enter the chest cavity.
- Complete absence of lung tissue.
- Narrowing of the bronchi.
8. During the canalicular stage of lung development, what significant event occurs?
- The formation of the laryngotracheal bud.
- The branching of the bronchi and bronchioles is complete.
- The respiratory bronchioles and alveolar ducts begin to form, and vascularization increases.
- Mature alveoli with thin walls are established.
9. Which disorder is characterized by chronic inflammation and narrowing of the airways, often triggered by allergens or irritants?
- Emphysema
- Cystic Fibrosis
- Asthma
- Bronchitis
10. The main muscle responsible for normal, quiet inspiration is the:
- External intercostals
- Internal intercostals
- Diaphragm
- Abdominal muscles
11. The smallest conducting airways in the lungs are called _____________.
12. The final stage of lung maturation, where mature alveoli with thin walls and close contact with capillaries are formed, is known as the _____________ stage.
13. A genetic disorder that causes thick, sticky mucus to build up in the lungs and other organs is _____________.
14. The vocal cords are located within the _____________.
15. _____________ is a condition where the lungs are incompletely developed or abnormally small.
Quiz Complete!
Your Score:
0%
0 / 0 correct