Menstruation: Preparing for pregnancy
The Menstrual Cycle
The menstrual cycle is a monthly series of natural changes in hormone production and the structures of the uterus and ovaries. It is a complex, coordinated process that prepares the female body for the possibility of pregnancy.
Averaging around 28 days, the cycle is designed to produce and release an egg (ovulation) and prepare the uterus for potential implantation. If pregnancy does not occur, the uterine lining is shed, resulting in menstruation.
Key Organs & Hormones Involved
The entire cycle is a masterful conversation between the brain and the reproductive organs, regulated by a precise cascade of hormones.
Hypothalamus
Releases GnRH to start the cascade.
Pituitary Gland
Releases FSH & LH to stimulate the ovaries.
Ovaries
Mature eggs; produce Estrogen & Progesterone.
Uterus
Its lining (endometrium) thickens and sheds.
The Purpose of the Cycle
The menstrual cycle is elegantly designed to ensure that if fertilization occurs, the uterus is perfectly prepared to nurture the developing embryo. If fertilization doesn't happen, the system resets itself, and the cycle begins anew, ready for the next opportunity.
Phases of the Menstrual Cycle
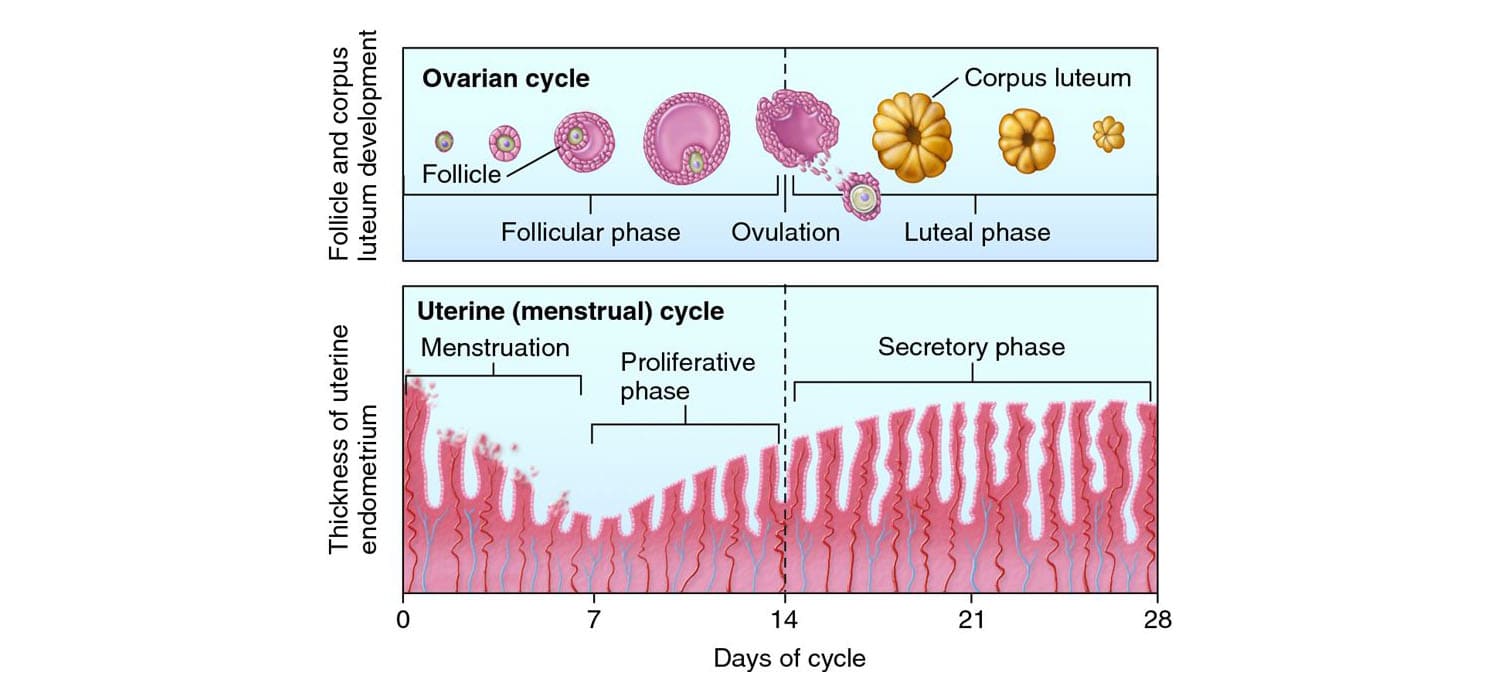
The entire process is best understood by looking at two main, overlapping cycles that happen simultaneously:
- The Ovarian Cycle: Focuses on what happens in the ovaries (egg maturation and release).
- The Uterine Cycle: Focuses on what happens in the uterus (preparation and shedding of the lining).
Let's explore these coordinated events in the next section.
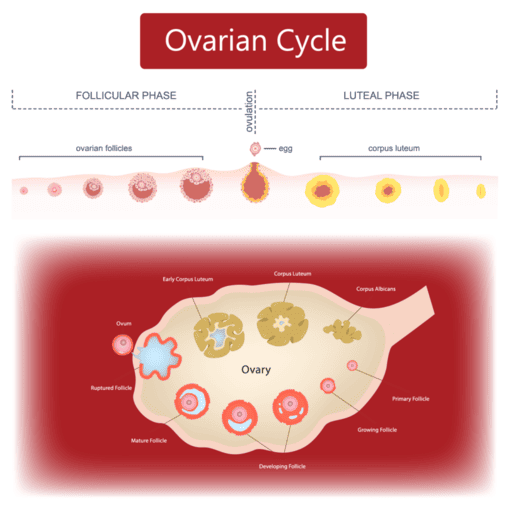
The Ovarian Cycle
This cycle describes the series of changes that occur within the follicles of the ovary, driven by fluctuating hormones. It is divided into three distinct phases.
A. The Follicular Phase (Day 1 to ~14)
What happens in the Ovary:
- Follicle Development: Under the influence of FSH, several primordial follicles begin to grow.
- Dominant Follicle Selection: Usually, only one follicle becomes the dominant (Graafian) follicle and continues to mature.
- Estrogen Production: The growing dominant follicle produces increasing amounts of estrogen.
Hormonal Control:
- FSH (Follicle-Stimulating Hormone): Stimulates initial follicle growth.
- Estrogen: Initially provides negative feedback on FSH, then switches to positive feedback, leading to the LH surge.
B. Ovulation (Around Day 14)
The Trigger:
The high surge of estrogen from the dominant follicle causes a sudden, dramatic release of Luteinizing Hormone (LH) from the pituitary gland (the "LH surge").
What happens in the Ovary:
The LH surge triggers the mature dominant follicle to rupture, expelling the secondary oocyte (arrested in Metaphase II) into the fallopian tube. The egg remains viable for fertilization for around 24 hours.
C. The Luteal Phase (~Day 14 to 28)
What happens in the Ovary:
- Corpus Luteum Formation: After ovulation, the ruptured follicle transforms into the corpus luteum ("yellow body").
- Hormone Production: The corpus luteum produces large amounts of progesterone and some estrogen.
- Fate of Corpus Luteum: It degenerates after 10-14 days if no pregnancy occurs. If pregnancy occurs, it is "rescued" by hCG to continue producing progesterone.
Hormonal Control:
- Progesterone: Becomes the dominant hormone, preparing the uterus for implantation.
- Negative Feedback: High progesterone and estrogen levels inhibit FSH and LH release, preventing new follicle development.
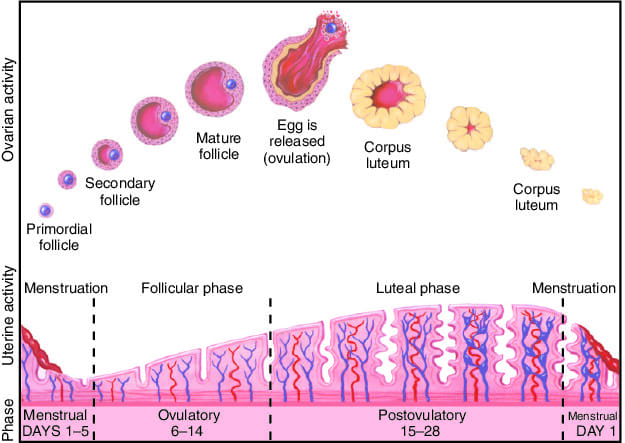
The Uterine Cycle
This cycle describes the corresponding changes occurring in the lining of the uterus (the endometrium). These changes are driven directly by the ovarian hormones, estrogen and progesterone, and are perfectly timed to coincide with the events of the ovarian cycle.
A. The Menstrual Phase (Day 1 to ~5-7)
What causes it:
This phase marks the start of the cycle (Day 1). The sharp drop in progesterone and estrogen from the degeneration of the previous cycle's corpus luteum causes the uterine lining to break down and shed, resulting in menstrual bleeding.
Purpose:
To clear out the old uterine lining, making way for a new cycle to begin.
B. The Proliferative Phase (~Day 5-7 to 14)
Driven by Estrogen:
Overlapping with the ovarian follicular phase, the rising estrogen from the dominant follicle stimulates the repair and regrowth of the endometrium.
What happens in the Uterus:
The endometrium thickens, and new blood vessels and glands develop, making the lining lush and ready to receive a fertilized egg.
C. The Secretory Phase (~Day 14 to 28)
Driven by Progesterone:
Overlapping with the ovarian luteal phase, this phase is primarily driven by the progesterone from the corpus luteum.
What happens in the Uterus:
The endometrium continues to thicken and its glands become highly secretory, producing nutrient-rich fluids (glycogen, mucus) to nourish a potential embryo and make the uterus receptive for implantation.
What Happens at the End of the Cycle?
There are two possible outcomes, which determine whether the cycle repeats or pauses.
If Pregnancy Does NOT Occur:
- The corpus luteum degenerates.
- Progesterone levels plummet.
- The uterine lining breaks down, and a new period begins at Day 1.
If Pregnancy Occurs:
- The implanted embryo produces hCG.
- hCG "rescues" the corpus luteum, keeping progesterone levels high.
- The uterine lining is maintained, the menstrual cycle pauses, and pregnancy is supported.
Test Your Knowledge
Check your understanding of the concepts covered in this post.
1. The ovarian cycle describes changes occurring in the __________, while the uterine cycle describes changes occurring in the ___________.
- Uterus; Ovary
- Ovary; Vagina
- Ovary; Uterus
- Uterus; Cervix
2. Which hormone is primarily responsible for initiating the development of ovarian follicles at the beginning of a new cycle?
- Estrogen
- Progesterone
- Luteinizing Hormone (LH)
- Follicle-Stimulating Hormone (FSH)
3. Ovulation typically occurs around day 14 of a 28-day cycle and is directly triggered by a surge in which hormone?
- Estrogen
- Progesterone
- Luteinizing Hormone (LH)
- Follicle-Stimulating Hormone (FSH)
4. During the proliferative phase of the uterine cycle, which event is happening?
- The functional layer of the endometrium is shed.
- The endometrium rebuilds itself under the influence of estrogen.
- Progesterone causes the endometrium to become highly vascularized and glandular.
- The corpus luteum is actively secreting progesterone.
5. Which ovarian structure primarily secretes progesterone after ovulation to prepare the uterus for potential implantation?
- Graafian follicle
- Primary follicle
- Corpus luteum
- Corpus albicans
6. If fertilization and implantation do not occur, the corpus luteum degenerates, leading to a drop in estrogen and progesterone levels. What is the immediate consequence of this hormonal drop on the uterus?
- Further thickening of the endometrium
- Onset of menstruation
- Ovulation
- Secretion of Human Chorionic Gonadotropin (hCG)
7. The follicular phase of the ovarian cycle corresponds to which phase(s) of the uterine cycle?
- Menstrual phase only
- Secretory phase only
- Menstrual and Proliferative phases
- Proliferative and Secretory phases
8. High levels of estrogen during the late follicular phase exert what kind of feedback on the hypothalamus and anterior pituitary, leading to the LH surge?
- Negative feedback
- Positive feedback
- No feedback
- Inhibitory feedback
9. What is the primary role of progesterone during the secretory phase of the uterine cycle?
- To cause the shedding of the endometrium.
- To stimulate the growth of new ovarian follicles.
- To maintain and enhance the vascularization and glandular activity of the endometrium, making it receptive to implantation.
- To trigger ovulation.
10. What is the main event that marks the beginning of the menstrual phase of the uterine cycle?
- Ovulation
- Implantation of a fertilized egg
- Degeneration of the corpus luteum
- Shedding of the functional layer of the endometrium
11. The entire cycle of changes in the uterus, encompassing the menstrual, proliferative, and secretory phases, is collectively known as the _____________.
12. The primary ovarian event during the secretory phase of the uterine cycle is the active presence and hormonal secretion of the _____________.
13. The release of the oocyte from the ovary is specifically called _____________.
14. If pregnancy occurs, the developing embryo produces the hormone _____________, which signals the corpus luteum to continue producing progesterone, thus maintaining the uterine lining.
15. During the early follicular phase, the rising levels of estrogen exert a ___________ feedback on the release of FSH and LH, preventing the development of too many follicles.
Quiz Complete!
Your Score:
0%
0 / 0 correct