Epithelium: The Body's Lining & Covering Tissue
What is Epithelium?
Epithelium forms continuous sheets of cells that line internal surfaces and cover the external surface of the body. It acts as a selective barrier that protects tissues and is often involved in absorption or secretion. A non-cellular layer called the basement membrane separates an epithelium from the underlying connective tissue.
Key Characteristics:
Anchorage & Polarity
Cells are anchored to a basement membrane and have an apical surface (facing a free space) and a basal surface (attached to the basement membrane).
Avascularity & Cellularity
Epithelium contains no blood vessels (avascular) and is composed almost entirely of tightly packed cells with very little extracellular matrix (cellularity).
Origin of the Epithelial Tissues
Epithelial tissues are diverse in function and location, which is reflected in their origins from all three primary germ layers formed during embryonic development. These are the primary layers of cells from which all tissues and organs of the body are derived.
Ectoderm (Outermost layer)
Gives rise to structures that interact with the outside world and the nervous system.
Epithelial Derivatives:
- Epidermis of the skin
- Lining of the oral & nasal cavities
- Lining of the anal canal
- Glands derived from skin
Mesoderm (Middle layer)
Forms structures related to movement, support, and circulation.
Epithelial Derivatives:
- Endothelium (lining blood vessels)
- Mesothelium (lining serous cavities)
- Epithelium of kidney tubules
- Epithelium of the gonads
Endoderm (Innermost layer)
Forms the lining of the digestive and respiratory systems and associated glands.
Epithelial Derivatives:
- Lining of the GI tract
- Lining of the respiratory tract
- Lining of the urinary bladder
- Epithelium of thyroid, pancreas, liver
The Basement Membrane
The basement membrane (BM) is a thin, acellular, extracellular layer that underlies all epithelial tissues, separating them from the adjacent connective tissue. It is a critical structural and functional component.
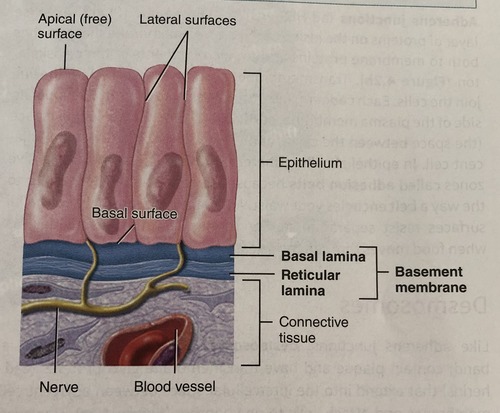
Composition & Structure
The BM is primarily composed of glycoproteins (like laminin), proteoglycans, and various types of collagen (especially Type IV collagen). Under an electron microscope, it is seen to have two main layers:
- Basal Lamina: Produced by the epithelial cells. It has a clearer layer (lamina lucida) and a denser layer (lamina densa).
- Reticular Lamina: Produced by the underlying connective tissue. It is composed of reticular fibers (Type III collagen) that anchor the basal lamina.
Functions of the Basement Membrane
Summary of Key Characteristics
- Anchored to basement membrane
- Apical and Basal surfaces (Polarity)
- No extracellular matrix (Cellularity)
- Avascular (no blood vessels)
Clinical Correlation: Invasion and Cancer
The basement membrane is a critical marker in cancer diagnosis. Benign tumors remain confined above the BM. A hallmark of malignant tumors (cancer) is their ability to produce enzymes that degrade the BM, allowing them to invade the underlying connective tissue and metastasize (spread).
Classification of Epithelium
Epithelium is classified based on two main features: the number of cell layers and the shape of the cells at the apical (free) surface.
Simple Squamous
Function: Ideal for diffusion and filtration. | Location: Alveoli of the lungs, lining of blood vessels (endothelium).
Simple Cuboidal
Function: Secretion and absorption. | Location: Kidney tubules, glands.
Simple Columnar
Function: Absorption and secretion. | Location: Gastrointestinal tract.
Stratified Squamous
Function: Protection against abrasion.
Transitional (Urinary) Epithelium
Function: Allows for distension (stretching). | Location: Urinary bladder, ureters.
Pseudostratified Ciliated Columnar (Respiratory) Epithelium
Function: Secretion and movement of mucus. | Location: Trachea, bronchi.
Simple squamous epithelium
Simple squamous epithelium is a single layer of thin, flattened cells that forms a delicate lining in areas where rapid diffusion, filtration, or smooth movement of substances is needed. The extreme thinness of the cells provides minimal protection but allows for quick transport of molecules.
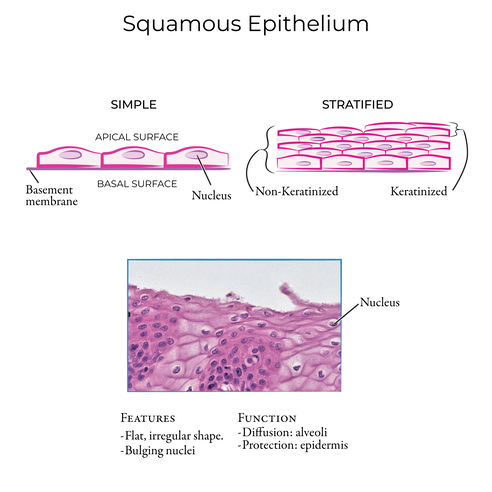
Classification & Defining Characteristics
Simple
Consists of a single layer of cells, crucial for rapid transport across the membrane.
Squamous
Cells are flat, thin, and scale-like ("squashed"), resembling a tiled floor from the surface.
Permeable
The extreme thinness of the single layer makes it highly permeable for quick exchange.
Structure & Appearance
- Cell Shape: Irregularly shaped, flattened cells that interlock like puzzle pieces.
- Nucleus: Oval or flattened, often appearing as a central bulge in the thin cell.
- Cytoplasm: Scanty (very little), reflecting its primary role in passive transport.
- Basement Membrane: Rests on a thin basement membrane, separating it from underlying connective tissue.
Locations and Functions
Simple squamous epithelium is strategically located in areas where rapid diffusion, filtration, or a slick, friction-reducing surface is required.
Lining of Blood & Lymphatic Vessels (Endothelium)
Provides a smooth, clot-preventing surface for blood flow and facilitates the exchange of gases, nutrients, and waste.
Lining of Serous Cavities (Mesothelium)
Lines the pleura, pericardium, and peritoneum, producing a slippery serous fluid that lubricates organs and prevents friction.
Alveoli of the Lungs (Type I Pneumocytes)
Forms the extremely thin "air-blood barrier" essential for rapid gas exchange (oxygen in, carbon dioxide out).
Glomerular Capsules (Bowman's Capsule) in the Kidneys
Forms the filtration membrane for blood, allowing water and small solutes to pass into the renal tubule while retaining large molecules.
Clinical Significance
Understanding the structure of simple squamous epithelium is key to diagnosing and managing several clinical conditions.
Pathological Considerations
- Edema: Fluid accumulation (e.g., in heart failure) increases the diffusion distance across the alveolar epithelium, impairing gas exchange.
- Inflammation: Inflammation of serous membranes (pleuritis, peritonitis) causes fluid accumulation (effusions) and painful friction.
- Cancer: Malignant mesotheliomas can arise from the mesothelium, and a disrupted endothelium is a key factor in various vascular diseases.
Simple cuboidal epithelium
Simple cuboidal epithelium is a single layer of cube-shaped cells, often with round, central nuclei, primarily performing secretion and absorption. It is found lining surfaces like kidney tubules, ducts of glands, and the surface of the ovary, where it plays a vital role in regulating substances and producing secretions.
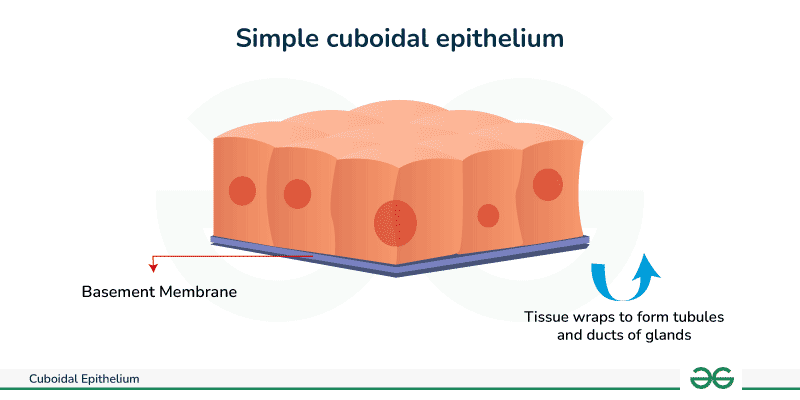
Classification & Defining Characteristics
Simple
Consists of a single layer of cells, allowing for controlled secretion and absorption.
Cuboidal
Cells are cube-like in shape, with a height and width that are approximately equal in cross-section.
Central Nucleus
The nucleus is spherical and centrally located, a key identifying feature.
Structure & Appearance
- Overall Shape: Forms a single layer of cells that often line a duct or tubule, encircling a central lumen (open space).
- Cytoplasm: Contains more cytoplasm and organelles than squamous cells, reflecting its active role in secretion and absorption.
- Specializations: The apical surface may have microvilli (a "brush border") to increase surface area, especially in the kidney tubules.
Locations and Functions
Simple cuboidal epithelium is found in locations primarily involved in secretion, absorption, and transport.
1. Kidney Tubules
Highly active in the absorption of water and nutrients from filtrate back into the blood, and secretion of waste products into the filtrate.
2. Small Ducts of Glands
Found in salivary glands, pancreas, and liver. Also forms the follicles of the thyroid gland, where it synthesizes and secretes thyroid hormones.
3. Ovary Surface (Germinal Epithelium)
Provides a protective covering for the surface of the ovary.
4. Choroid Plexus of the Brain
Specialized cuboidal cells that produce cerebrospinal fluid (CSF).
Clinical Significance
Dysfunction of simple cuboidal epithelium is linked to several significant diseases.
Pathological Considerations
- Polycystic Kidney Disease (PKD): A genetic disorder where cysts lined by abnormal cuboidal cells form in the kidneys, leading to kidney failure.
- Glandular Dysfunction: Thyroid disorders often involve altered function of the simple cuboidal cells that form the secretory follicles.
- Carcinomas: Cancers originating from glandular tissue (adenocarcinomas), such as renal cell carcinoma, arise from these epithelial cells.
Simple columnar epithelium
Simple columnar epithelium is a single layer of tall, column-shaped cells lining organs like the stomach and intestines. These cells are highly specialized for absorption and secretion, featuring nuclei located near the basement membrane and often possessing apical specializations like microvilli or cilia.
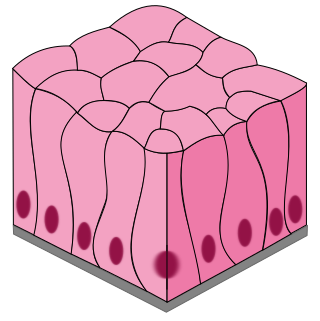
Classification & Defining Characteristics
- Simple: A single layer of cells, maximizing efficiency for absorption and secretion.
- Columnar: The cells are distinctly taller than they are wide, providing ample cytoplasmic volume for metabolic machinery.
- Basal Nucleus: The nucleus is typically oval-shaped and located basally (closer to the basement membrane), a key diagnostic feature.
Key Specializations
This is where simple columnar epithelium truly excels, often having specialized apical modifications to enhance its functions:
Microvilli (Brush Border)
Minute, finger-like projections that vastly increase surface area for absorption. Found in the small intestine.
Cilia
Longer, motile projections that propel substances along the surface. Found in uterine (fallopian) tubes.
Goblet Cells
Specialized unicellular glands that secrete mucus for lubrication and protection. Abundant in the GI tract.
Locations and Functions
Simple columnar epithelium is found in areas demanding high levels of absorption, secretion, and sometimes transport.
Gastrointestinal Tract (Stomach to Rectum)
In the stomach, it secretes mucus and enzymes. In the small intestine, it is the primary site for nutrient absorption, enhanced by microvilli. In the large intestine, it absorbs water and secretes mucus.
Gallbladder
Primarily for water absorption to concentrate bile. Contains microvilli but no goblet cells.
Uterine (Fallopian) Tubes
Contains ciliated columnar cells that help propel the ovum towards the uterus.
Clinical Significance
Damage or changes to simple columnar epithelium are central to many significant diseases, particularly in the gastrointestinal tract.
Pathological Considerations
- Malabsorption Syndromes: In Celiac Disease, damage to the intestinal columnar epithelium flattens microvilli, drastically reducing nutrient absorption.
- Metaplasia (Barrett's Esophagus): Chronic acid reflux can cause the esophageal lining to change into a columnar type, a precancerous condition.
- Adenocarcinomas: Cancers arising from glandular tissue, like colorectal cancer, originate from simple columnar epithelium.
- Cystic Fibrosis: Affects mucus-secreting goblet cells, producing abnormally thick mucus that impairs clearance in the respiratory tract and blocks ducts.
Stratified squamous epithelium
Stratified squamous epithelium is a protective tissue composed of multiple layers of cells, with flattened, scale-like cells at the surface. Its primary function is to provide a physical barrier against abrasion, microorganisms, and water loss. It is the most common type of stratified epithelium in the body.
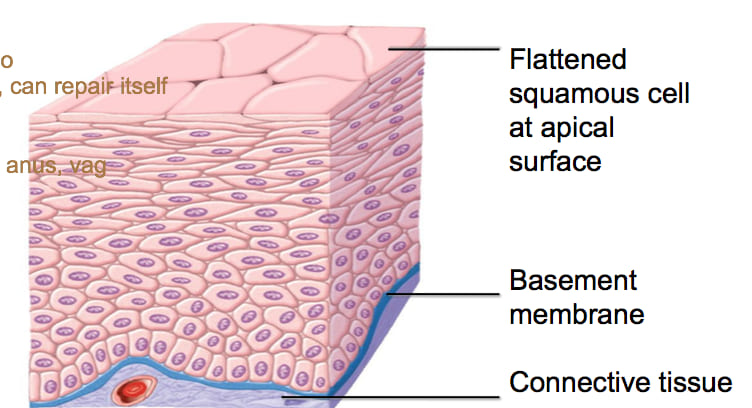
Classification & Defining Characteristics
- Stratified: Consists of multiple layers of cells, providing robust protection.
- Squamous: The cells in the most superficial (apical) layer are flat and scale-like. The classification name is always based on this top layer.
- Basal Layer: The deepest (basal) layer consists of cuboidal or columnar cells that are actively mitotic, constantly producing new cells that are pushed towards the surface.
Layers and Structure
The tissue is organized into distinct layers, from the actively dividing basal layer to the flattened superficial layer.
- Basal Layer (Stratum Basale): A single layer of cuboidal/columnar stem cells resting on the basement membrane.
- Intermediate Layers: Cells become more polyhedral and then progressively flatter as they are pushed upwards. They are strongly connected by numerous desmosomes.
- Superficial Layer: Composed of flattened, squamous cells, which are eventually shed from the surface.
The Two Main Subtypes
Stratified squamous epithelium is further divided based on the presence or absence of a key protein—keratin—in its superficial layers.
A. Keratinized Stratified Squamous
The most superficial layers are composed of dead cells filled with keratin, a tough, water-resistant protein. These cells lack nuclei.
Key Features & Locations:
- Appearance: Dry, flaky surface.
- Function: Waterproofing, protection from abrasion and pathogens.
- Location: Epidermis of the skin.
B. Non-Keratinized Stratified Squamous
The superficial cells do not contain significant keratin and remain alive, retaining their nuclei.
Key Features & Locations:
- Appearance: Moist surface.
- Function: Protection against abrasion in moist areas.
- Locations: Oral cavity, esophagus, vagina, anal canal.
Clinical Significance
As a primary protective barrier, this epithelium is central to many disease processes and clinical assessments.
Pathological Considerations
- Psoriasis: Hyperproliferation and abnormal keratinization of the epidermis, leading to thick, scaly plaques.
- Cancer: A high percentage of human cancers (e.g., squamous cell carcinoma of the skin, mouth, cervix) originate from this tissue. A Pap smear checks for precancerous changes in the cervical epithelium.
- Leukoplakia: A precancerous condition involving the thickening of non-keratinized epithelium (e.g., in the mouth) due to chronic irritation like tobacco use.
Transitional epithelium
Transitional epithelium, also known as urothelium, is a specialized, multi-layered type of stratified epithelium found exclusively in the urinary system. Its most remarkable feature is its ability to stretch and recoil, allowing organs like the bladder to expand significantly without losing structural integrity or allowing the toxic components of urine to leak into underlying tissues.

Classification & Defining Characteristics
While stratified, its key feature is its ability to change shape, or "transition," based on the degree of stretch.
Relaxed / Contracted State
Appears to have 4-6+ layers. The most superficial (apical) cells are large, dome-shaped, and often bi-nucleated. These are known as "umbrella cells."
Distended / Stretched State
The entire epithelial layer thins to just 2-3 layers. The umbrella cells flatten out, becoming more squamous-like in appearance to accommodate the increased volume.
Umbrella Cells & Impermeability
The large, outermost umbrella cells are highly specialized. They have a thickened apical plasma membrane, sometimes called a "crust," formed by specialized proteins called uroplakins. This unique feature makes the epithelium impermeable, forming a crucial barrier that protects the underlying cells from the hypertonic and toxic effects of urine.
Locations and Functions
Transitional epithelium is exclusively found lining the hollow organs of the urinary tract:
Clinical Significance
As the primary lining of the urinary tract, urothelium is central to many common and serious urological conditions.
Pathological Considerations
- Bladder Cancer (Urothelial Carcinoma): The vast majority of cancers of the bladder, ureters, and renal pelvis originate from this tissue. Smoking is a major risk factor.
- Urinary Tract Infections (UTIs): Pathogens like E. coli can adhere to and invade urothelial cells, leading to infections.
- Cystitis: Inflammation of the bladder lining due to infection or irritation, leading to symptoms like pain, urgency, and frequency.
Pseudostratified columnar epithelium
Pseudostratified columnar epithelium is a single layer of cells that appears multi-layered because the nuclei are at different heights, though all cells are anchored to the basement membrane. It is found in areas like the trachea and upper respiratory tract, where it often bears cilia to move mucus.
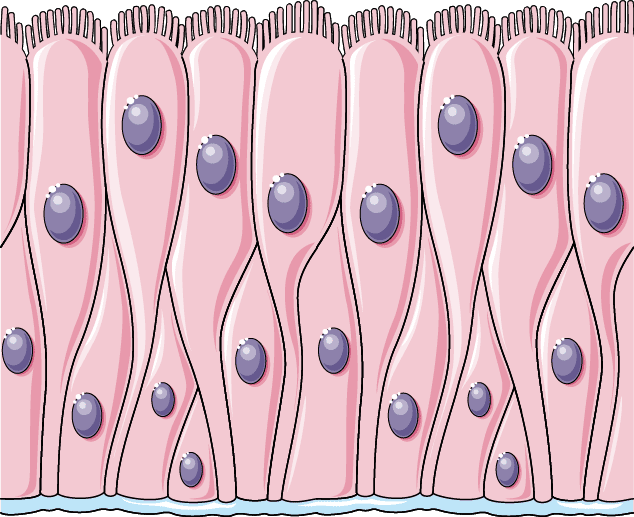
Classification & Defining Characteristics
- Pseudostratified: The key feature. It appears stratified because its nuclei are at different levels, but it is a single layer as all cells touch the basement membrane.
- Columnar: The cells that reach the apical surface are tall and column-shaped.
- Ciliated: The surface cells typically possess numerous motile, hair-like cilia.
- Goblet Cells: Almost always contains numerous interspersed goblet cells that secrete mucus.
Structure & Cell Types
This "crowded" arrangement gives the illusion of stratification and contains three main cell types:
Columnar Ciliated Cells
Tall cells that reach the surface and bear the motile cilia.
Goblet Cells
Mucus-secreting unicellular glands interspersed among the other cells.
Basal Cells
Small stem cells that sit on the basement membrane and regenerate the other cell types.
Locations and Functions
This highly specialized epithelium is almost exclusively found in the respiratory tract, where it performs its vital role in the "mucociliary escalator."
The Mucociliary Escalator
This is its most famous function. Goblet cells produce a sticky layer of mucus that traps inhaled dust, pollen, and pathogens. The cilia then beat in a coordinated rhythm, sweeping the mucus upwards towards the pharynx, where it can be swallowed or expelled. This prevents foreign substances from reaching the delicate lung tissue.
Key Locations:
- Nasal Cavity, Paranasal Sinuses, Nasopharynx
- Trachea and Bronchi (large and medium-sized)
- Exception: In the Epididymis, it has immotile stereocilia and functions in absorption for sperm maturation.
Clinical Significance
As the first line of defense against airborne pathogens, dysfunction of this epithelium has severe consequences for respiratory health.
Pathological Considerations
- Smoking: Chronic smoking paralyzes and destroys cilia, compromising the mucociliary escalator and leading to mucus buildup, chronic bronchitis, and increased infection risk.
- Squamous Metaplasia: Due to chronic irritation (like smoking), this tissue can change into stratified squamous epithelium. While more protective, it lacks cilia and goblet cells, losing the vital escalator function and increasing the risk of cancer.
- Cystic Fibrosis: A genetic disease causing abnormally thick mucus that impairs ciliary function, clogs airways, and leads to chronic respiratory infections.
- Kartagener Syndrome (PCD): A genetic disorder causing defective, immotile cilia, leading to chronic respiratory infections and male infertility.
Glandular Epithelium
Glandular epithelium is a specialized tissue composed of cells whose primary function is secretion. These cells are highly specialized to synthesize, store, and release substances such as hormones, mucus, enzymes, and sweat. All glands in the body develop from ingrowths of epithelial sheets into the underlying connective tissue.
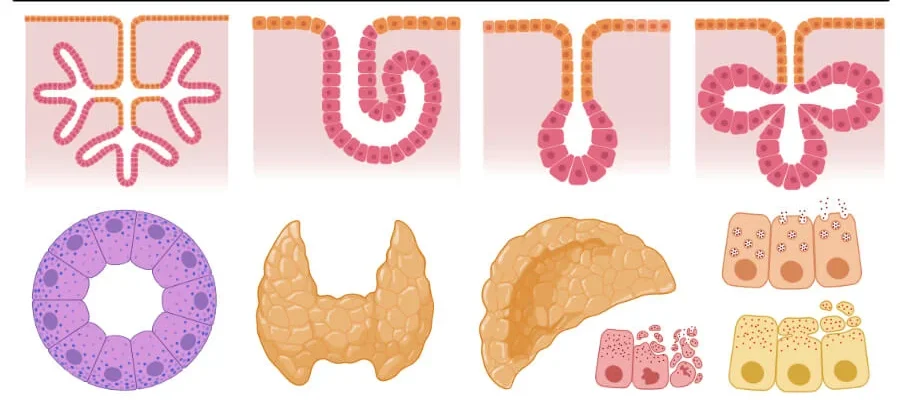
Classification of Glands
Glands are primarily classified based on where they release their secretions:
A. Exocrine Glands (External Secretion)
Secrete their products onto an epithelial surface, either directly or through a duct.
Examples:
- Sweat glands
- Salivary glands
- Pancreas (exocrine portion)
- Mammary glands
- Sebaceous (oil) glands
B. Endocrine Glands (Internal Secretion)
Secrete their products (hormones) directly into the bloodstream. They are ductless.
Examples:
- Thyroid gland
- Adrenal glands
- Pituitary gland
- Pancreas (endocrine islets)
- Ovaries & Testes
Modes of Exocrine Secretion
Exocrine glands release their products in three different ways:
Merocrine (Eccrine)
Secretion via exocytosis with no loss of cytoplasm. (Most common)
Apocrine
A portion of the apical cytoplasm pinches off with the secretion.
Holocrine
The entire cell ruptures to release its contents, leading to cell death.
Types of Secretion
- Serous: A watery fluid, often rich in enzymes (e.g., parotid salivary gland).
- Mucous: A viscous, sticky fluid (mucus) for lubrication and protection (e.g., goblet cells).
- Mixed: Produce both serous and mucous secretions (e.g., submandibular salivary gland).
Clinical Significance
The health and function of glandular epithelium are central to many physiological processes and disease states.
Pathological Considerations
- Glandular Dysfunction: Many diseases involve hypo- or hyperfunction. Exocrine examples include Cystic Fibrosis (abnormal mucus). Endocrine examples include Diabetes (pancreas) and Thyroid disorders.
- Tumors/Cancers: Many cancers originate from glandular epithelium. Benign tumors are called adenomas, and malignant cancers are called adenocarcinomas (e.g., breast, colon, prostate cancer).
- Inflammation (Adenitis): Inflammation of glands, such as sialadenitis (salivary glands) or mastitis (mammary glands).
Test Your Knowledge
Check your understanding of the concepts covered in this post.
1. Which of the following is a general characteristic of epithelial tissue?
- Contains abundant extracellular matrix.
- Always highly vascularized.
- Cells are closely packed with little intercellular space.
- Primarily specialized for contraction.
2. Where would you most likely find simple squamous epithelium?
- Lining the stomach and intestines.
- Forming the outer layer of the skin.
- Lining blood vessels (endothelium) and lung alveoli.
- In the ducts of large glands.
3. A tissue consisting of multiple layers of cells, with the top layer being flat and squamous, would be classified as:
- Simple cuboidal epithelium.
- Stratified columnar epithelium.
- Pseudostratified columnar epithelium.
- Stratified squamous epithelium.
4. Which type of epithelium is characterized by a single layer of cells of varying heights, all attached to the basement membrane, but not all reaching the free surface, often possessing cilia and goblet cells?
- Simple columnar epithelium.
- Stratified cuboidal epithelium.
- Pseudostratified columnar epithelium.
- Transitional epithelium.
5. Glands that secrete their products directly into the bloodstream (ductless glands) are classified as:
- Exocrine glands.
- Endocrine glands.
- Merocrine glands.
- Apocrine glands.
6. Which statement correctly describes transitional epithelium?
- It is found in the lining of the stomach and secretes digestive enzymes.
- It allows for stretching and distension, found in the urinary bladder.
- It is a single layer of tall, narrow cells with microvilli, found in the intestines.
- It forms the protective outer layer of the skin.
7. A gland that releases its secretory product by exocytosis, without any loss of glandular cell cytoplasm, is classified as a:
- Holocrine gland.
- Apocrine gland.
- Merocrine gland.
- Sebaceous gland.
8. Goblet cells are unicellular glands commonly found within which type of epithelium, where they secrete mucus?
- Stratified squamous epithelium.
- Simple cuboidal epithelium.
- Pseudostratified and simple columnar epithelium.
- Simple squamous epithelium.
9. Which type of epithelial tissue is best adapted for absorption and secretion, often featuring microvilli on its apical surface?
- Simple squamous epithelium.
- Simple cuboidal epithelium.
- Simple columnar epithelium.
- Stratified cuboidal epithelium.
10. A gland whose entire cell ruptures to release its secretory product (along with dead cell fragments) is a:
- Merocrine gland.
- Apocrine gland.
- Holocrine gland.
- Endocrine gland.
11. All epithelial tissues are attached to an underlying connective tissue layer by a non-cellular layer called the ________________.
12. Epithelial tissue is described as ________________ because it lacks direct blood vessels and receives nutrients by diffusion.
13. The type of epithelial tissue that forms the epidermis of the skin, providing protection against abrasion, is ________________ squamous epithelium.
14. Glands that secrete their products into ducts, which then carry the secretions to an epithelial surface, are known as ________________ glands.
15. The kidney tubules are typically lined by a single layer of cube-shaped cells, making this tissue type ________________ cuboidal epithelium.
Quiz Complete!
Your Score:
0%
0 / 0 correct