Respirator System Anatomy: Breath in, Out!
Objective: To describe the macroscopic and microscopic anatomy of the respiratory system and relate structure to function in the processes of air conduction, gas exchange, and protection.
Introduction to the Respiratory System
The respiratory system is a complex network of organs and tissues that work together to move air into and out of the body and facilitate gas exchange. It can be broadly divided into two main parts based on function: the conducting zone (for air transport) and the respiratory zone (for gas exchange).
The respiratory system is a vital biological system responsible for the exchange of gases between the body and the external environment. Its primary function is to take in oxygen (O₂) from the atmosphere and expel carbon dioxide (CO₂), a waste product of cellular metabolism. This process, known as respiration, is essential for energy production and maintaining the body's pH balance.
A. Upper Respiratory Tract (Conducting Zone)
This part of the system is primarily involved in conditioning the inspired air.
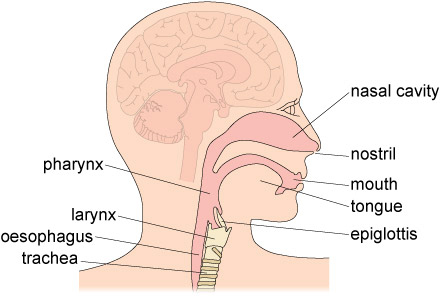
1. Nose and Nasal Cavity
- External Nose: The visible part, supported by bone and cartilage.
- Nasal Cavity: Extends from the nostrils (nares) to the posterior nasal apertures (choanae).
- Vestibule: The anterior-most part, lined with skin and stiff hairs (vibrissae) that filter large particles.
- Nasal Conchae (Turbinates): Three bony projections (superior, middle, inferior) covered by mucous membranes. They dramatically increase the surface area of the nasal cavity and create turbulent airflow.
Function of Turbinates & Mucosa
This turbulent flow forces inhaled air to come into contact with the moist mucous membranes, which effectively:
- Filters: Traps dust, pollen, and other particulate matter.
- Warms: Heat from the underlying capillaries warms the air to body temperature.
- Humidifies: Water vapor from the mucus moistens the air, preventing drying of the delicate lung tissues.
Mucosal Types:
- Olfactory Mucosa: Located in the superior nasal cavity; contains olfactory receptors for the sense of smell.
- Respiratory Mucosa: Lines most of the nasal cavity; composed of pseudostratified ciliated columnar epithelium with abundant goblet cells.
- Goblet Cells: Produce mucus.
- Cilia: Beat rhythmically to move mucus (and trapped particles) towards the pharynx to be swallowed. This is part of the mucociliary escalator.
Paranasal Sinuses: Air-filled cavities in the frontal, sphenoid, ethmoid, and maxillary bones. They lighten the skull, warm and humidify air, and contribute to voice resonance. They drain into the nasal cavity.
2. Pharynx (Throat)
A muscular tube extending from the posterior nasal cavity to the esophagus and larynx. It serves as a passageway for both air and food.
Regions:
- Nasopharynx: Posterior to the nasal cavity. Lined with pseudostratified ciliated columnar epithelium. Contains the pharyngeal tonsils (adenoids) and the openings of the auditory (Eustachian) tubes.
- Oropharynx: Posterior to the oral cavity. Lined with stratified squamous epithelium (to resist abrasion from food). Contains the palatine and lingual tonsils.
- Laryngopharynx: Extends from the epiglottis to the esophagus. Also lined with stratified squamous epithelium.
Function: Passageway for air and food; voice resonance; protective immune function (tonsils).
3. Larynx (Voice Box)
Connects the pharynx to the trachea. Primarily cartilaginous structure.
Main Cartilages
- Thyroid Cartilage: The largest, forms the "Adam's apple."
- Cricoid Cartilage: Ring-shaped, inferior to the thyroid cartilage, forms the base of the larynx.
- Epiglottis: Leaf-shaped elastic cartilage that guards the glottis (opening to the larynx). During swallowing, it tips posteriorly to prevent food from entering the trachea.
- Arytenoid, Corniculate, Cuneiform: Small cartilages involved in vocal cord movement.
Vocal Folds & Function
Vocal Folds (True Vocal Cords): Ligaments covered by mucous membrane, stretching across the larynx. Vibrate to produce sound as air passes over them. Tension is controlled by small intrinsic muscles.
Functions:
- Air passageway: Keeps the airway open.
- Voice production (phonation).
- Prevention of food/liquid aspiration: Epiglottis and vocal cord closure.
B. Lower Respiratory Tract (Conducting and Respiratory Zones)
This part begins in the neck and extends into the thoracic cavity, leading to the lungs.
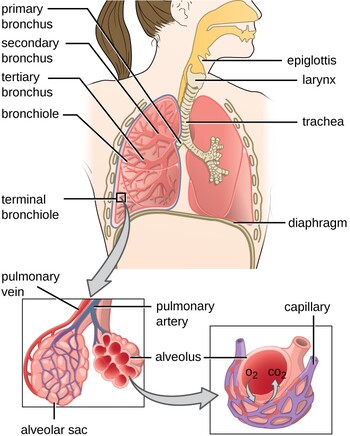
1. Trachea (Windpipe)
A rigid tube extending from the larynx (C6) to the main bronchi (T4/T5, carina).
- Structure: Composed of 16-20 C-shaped rings of hyaline cartilage.
- Function of Cartilage Rings: Prevent tracheal collapse, ensuring a patent airway. The open posterior ends of the C-rings are connected by the trachealis muscle, allowing the esophagus to expand anteriorly during swallowing.
- Lining: Similar to the nasal cavity, it is lined with pseudostratified ciliated columnar epithelium with goblet cells, forming a robust mucociliary escalator that traps and sweeps debris upwards towards the pharynx.
- Carina: The point where the trachea bifurcates into the left and right main bronchi. This area is highly sensitive, and touching it triggers a strong cough reflex.
2. Bronchi
The trachea divides into two main (primary) bronchi, one for each lung.
Clinical Note: The right main bronchus is shorter, wider, and more vertical than the left, making it a more common site for aspirated foreign objects.
Within the lungs, the branching continues:
- Main bronchi divide into lobar (secondary) bronchi (three on the right, two on the left, corresponding to lung lobes).
- Lobar bronchi then divide into segmental (tertiary) bronchi (supplying bronchopulmonary segments).
- Structure: Bronchi maintain cartilage (initially rings, then irregular plates) to keep them open. They are also lined with pseudostratified ciliated columnar epithelium, though it gradually becomes shorter and less abundant deeper in the system. Smooth muscle becomes more prominent as cartilage diminishes.
3. Bronchioles
Bronchi continue to branch and become progressively smaller, eventually losing their cartilage support and becoming bronchioles (diameter < 1 mm).
- Terminal Bronchioles: The smallest airways of the conducting zone. Lined with simple cuboidal epithelium. They contain club cells (Clara cells), which secrete components of surfactant, detoxify airborne toxins, and act as stem cells.
- Function: These are primarily smooth muscle tubes, allowing for significant control over airway diameter and thus airflow resistance (bronchodilation and bronchoconstriction). The mucociliary escalator fades out here.
4. Respiratory Bronchioles & Alveolar Ducts
- Respiratory Bronchioles: The first part of the respiratory zone, where gas exchange can begin. Distinguished from terminal bronchioles by the presence of a few scattered alveoli in their walls. Lined with simple cuboidal epithelium.
- Alveolar Ducts: Branch off the respiratory bronchioles. They are essentially tubes composed of rings of alveoli.
- Alveolar Sacs: Clusters of alveoli at the ends of alveolar ducts, resembling a bunch of grapes. The primary site of gas exchange.
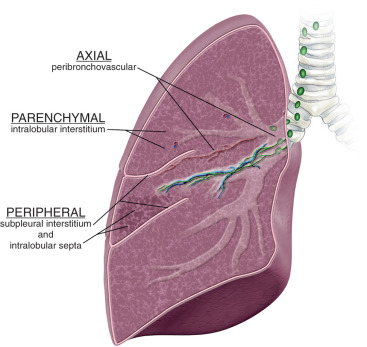
C. Lung Parenchyma
The functional tissue of the lungs, primarily composed of alveoli.
1. Alveoli (Air Sacs)
Tiny, thin-walled air sacs, numbering about 300-500 million per lung. They collectively provide an enormous surface area (approx. 70-100 m²) for gas exchange.
Type I Pneumocytes
(Squamous Alveolar Cells)
Extremely thin, flattened cells (0.1-0.5 µm thick). They form the primary structural component of the alveolar wall and are the main site of gas exchange. Their thinness minimizes diffusion distance.
Type II Pneumocytes
(Septal Cells)
Cuboidal cells interspersed among Type I cells. They secrete surfactant, a lipoprotein complex that reduces the surface tension of the alveolar fluid, preventing alveolar collapse during expiration. They can also differentiate into Type I pneumocytes to repair damaged alveolar lining.
Alveolar Macrophages
(Dust Cells)
Phagocytic cells that patrol the alveolar surface, engulfing dust, pathogens, and debris that enter the alveoli. They are essential for lung defense.
Elastic Fibers: The alveolar walls contain abundant elastic fibers, contributing to the elastic recoil of the lungs during expiration.
2. Alveolar-Capillary Membrane (Respiratory Membrane)
The thin barrier through which gas exchange occurs between the alveoli and the blood. It is extremely thin (0.2-0.6 µm), optimizing the diffusion rate.
Components (from air to blood):
- Layer of alveolar fluid containing surfactant.
- Alveolar epithelium (Type I pneumocyte).
- Fused basement membrane of the alveolar epithelium and capillary endothelium.
- Capillary endothelium.
Interstitium: The connective tissue space between the alveolar epithelial cells and the capillary endothelial cells. It contains collagen, elastic fibers, and some interstitial fluid. Its thickness can significantly impact gas diffusion in disease states.
D. Pleura
The lungs are enclosed in serous membranes called pleura.
- Visceral Pleura: Covers the surface of the lungs, dipping into the fissures between the lobes.
- Parietal Pleura: Lines the thoracic cavity wall, mediastinum, and superior surface of the diaphragm.
- Pleural Cavity: The potential space between the visceral and parietal pleura.
- Pleural Fluid: A thin layer of serous fluid (about
10-20 mL) within the pleural cavity.
- Lubrication: Allows the lungs to slide smoothly against the thoracic wall during breathing.
- Surface Tension (Adhesion): Creates an adhesive force that keeps the lung surface "stuck" to the thoracic wall, allowing the lungs to expand and recoil with the chest wall. This is crucial for maintaining the negative intrapleural pressure and facilitating lung expansion.
E. Respiratory Muscles
The muscles responsible for changing the volume of the thoracic cavity, thereby driving air movement.
Primary Muscles of Inspiration
A large, dome-shaped sheet of skeletal muscle separating the thoracic and abdominal cavities.
- Contraction: Flattens and moves inferiorly, increasing the vertical dimension of the thoracic cavity.
- Innervation: Phrenic nerves (C3-C5).
Located between the ribs.
- Contraction: Pulls the rib cage upwards and outwards, increasing the anteroposterior and lateral dimensions.
Expiration & Accessory Muscles
Located deep to the external intercostals. Primarily used in forced expiration.
- Contraction: Pulls the rib cage downwards and inwards, decreasing thoracic volume.
- Forced Inspiration: Sternocleidomastoid, scalenes, pectoralis minor.
- Forced Expiration: Abdominal muscles (rectus abdominis, internal and external obliques, transversus abdominis) – push abdominal contents upwards, forcing diaphragm up.
Key Functions of the Respiratory System
Gas Exchange
The exchange of O₂ and CO₂ between the lungs and blood (external) and between the blood and tissues (internal).
Ventilation (Breathing)
The mechanical process of moving air into (inhalation) and out of (exhalation) the lungs.
Acid-Base Balance
Regulates blood pH by controlling CO₂ levels in the blood.
Speech (Phonation)
Air passing over the vocal cords produces sound for vocalization.
Olfaction (Smell)
Olfactory receptors in the nasal cavity detect airborne chemicals.
Protection & Defense
Filters, warms, and humidifies inhaled air, trapping pathogens and irritants.
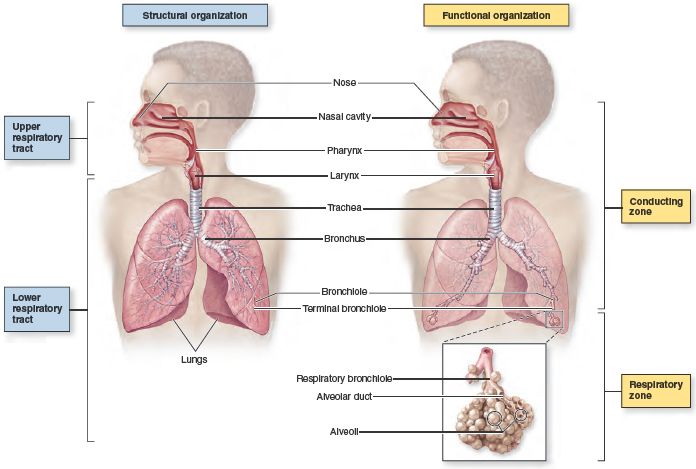
Organization of the Respiratory System
The system can be divided into two main zones based on function and anatomy.
Conducting Zone
A series of interconnected cavities and tubes that conduct, filter, warm, and humidify air on its way to the lungs. No gas exchange occurs here.
Components:
- Nasal Cavity & Pharynx
- Larynx & Trachea
- Bronchi & Terminal Bronchioles
Respiratory Zone
The site where the actual gas exchange between air and blood takes place. This is the functional end of the respiratory tract.
Components:
- Respiratory Bronchioles
- Alveolar Ducts & Sacs
- Alveoli
Components and Associated Structures
The respiratory system is a complex network of organs and structures that can be divided into upper and lower tracts.
Upper Respiratory Tract
Includes the nose, nasal cavity, pharynx (naso-, oro-, laryngo-), and larynx.
Lower Respiratory Tract
Includes the trachea, bronchi, bronchioles, and the lungs (containing the respiratory zone structures).
Associated Structures
- Thoracic Cage: Ribs, sternum, and thoracic vertebrae that form a protective bony framework.
- Respiratory Muscles: The diaphragm and intercostal muscles, responsible for the mechanics of breathing.
- Pleura: Membranes surrounding the lungs that facilitate smooth movement.
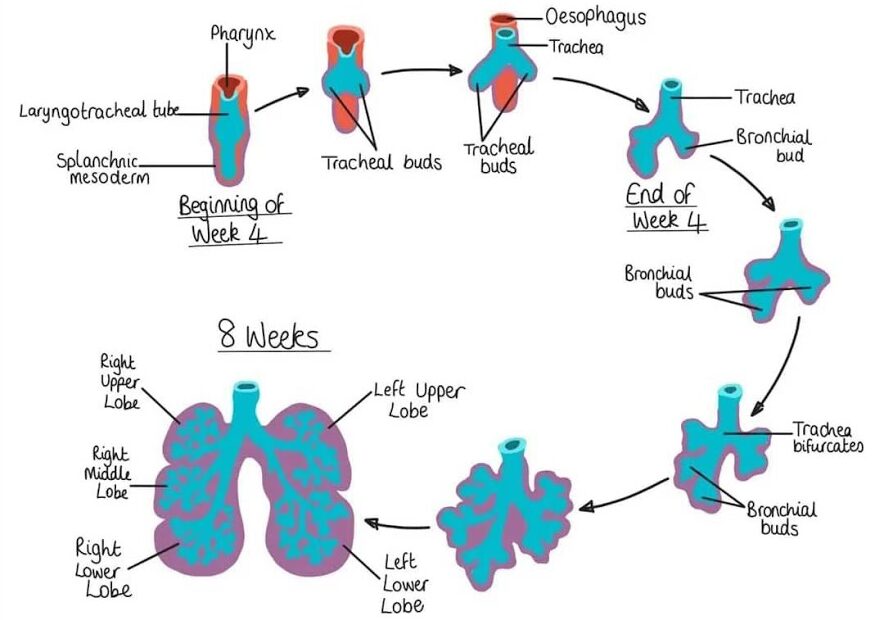
Respiratory System Development
The respiratory system begins its development early in embryonic life (around week 4) as a ventral outgrowth from the primitive foregut, highlighting its close developmental relationship with the digestive system.
1. Laryngotracheal Diverticulum (Respiratory Bud)
A groove in the ventral wall of the foregut deepens and grows outward to form the respiratory bud. This bud is then separated from the foregut by the fusion of the tracheoesophageal septum, forming the laryngotracheal tube (future respiratory tract) and the esophagus (digestive tract).
2. Larynx
The lining of the larynx develops from the endoderm of the cranial end of the tube. The cartilages and muscles are derived from the mesenchyme of the 4th and 6th pharyngeal arches. The lumen reopens (recanalization) to form the vocal cords.
3. Trachea
The trachea develops from the part of the tube distal to the larynx. Its epithelial lining and glands are from endoderm, while the cartilaginous rings, muscle, and connective tissue are from the surrounding splanchnic mesenchyme.
4. Bronchi and Lungs
Bronchial Buds & Branching:
Around week 5, the laryngotracheal tube bifurcates into two bronchial buds. These buds undergo a process called branching morphogenesis, repeatedly dividing to form the entire bronchial tree: primary, secondary (lobar), and tertiary (segmental) bronchi, and eventually the smaller bronchioles.
Tissue Origins:
- The entire epithelial lining of the bronchial tree and alveoli is derived from endoderm.
- The connective tissue, cartilage, smooth muscle, and blood vessels are derived from the surrounding splanchnic mesenchyme.
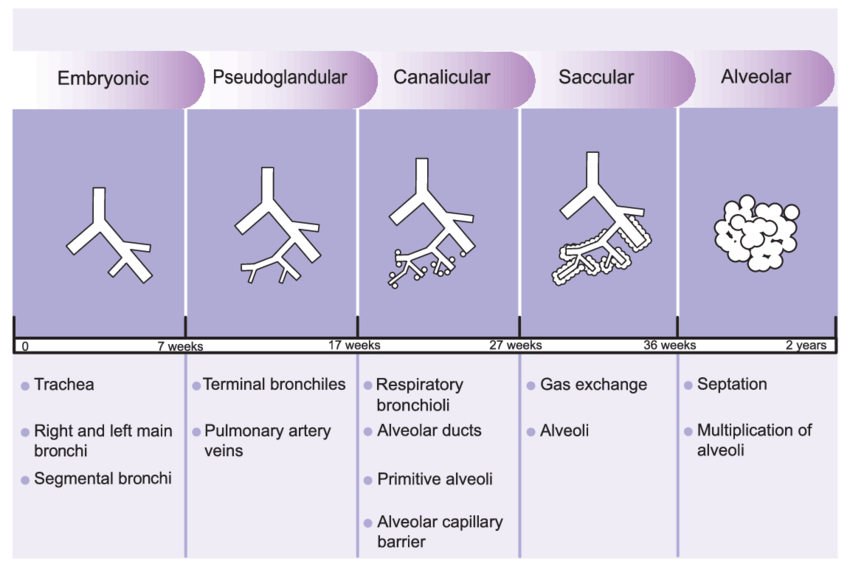
Maturation of the Lungs
The development of the lungs from simple tubes into a complex organ capable of gas exchange is a prolonged process that continues from early embryonic life until well after birth. This maturation can be divided into several distinct histological stages.
1. Embryonic Stage (Weeks 4-7)
This initial stage involves the formation of the laryngotracheal diverticulum and its division into the primary, secondary, and tertiary bronchi, establishing the basic framework of the tracheobronchial tree.
2. Pseudoglandular Stage (Weeks 5-16)
The bronchial tree undergoes extensive branching to form the terminal bronchioles. The lung tissue at this stage resembles a gland, hence the name. Crucially, no respiratory bronchioles or alveoli are present yet, so respiration is not possible.
3. Canalicular Stage (Weeks 16-26)
The terminal bronchioles divide into respiratory bronchioles, which then divide into alveolar ducts. The lung tissue becomes highly vascularized. Some primitive alveolar sacs (saccules) begin to form. Survival is difficult, but some gas exchange may be possible near the end of this stage.
4. Saccular Stage (Weeks 26-Birth)
Alveolar ducts terminate in thin-walled terminal sacs (saccules). Two crucial cell types differentiate: Type I pneumocytes (for gas exchange) and Type II pneumocytes, which begin to produce surfactant. Surfactant is essential for reducing surface tension and preventing the collapse of the air sacs during exhalation.
5. Alveolar Stage (Late Fetal to ~8 Years)
Mature alveoli develop from the saccules. The number of alveoli continues to increase significantly after birth, from about 50 million at birth to the adult number of approximately 300 million by 8 years of age. This highlights that lung development is a long postnatal process.
Summary of Tissue Origins
A recap of the germ layers responsible for forming the respiratory system:
- Endoderm: Forms the entire epithelial lining of the larynx, trachea, bronchi, and alveoli, as well as the glands.
- Splanchnic Mesenchyme: Forms all the supporting structures, including the cartilage, smooth muscle, connective tissue, and blood vessels of the respiratory tract.
The Pleura and its Nerve Supply
The pleura are serous membranes that envelop the lungs and line the walls of the thoracic cavity. They play a critical role in lung function by allowing smooth movement during breathing and creating the necessary pressure environment for lung inflation.
A. The Pleural Layers
Visceral Pleura
This layer directly covers the entire surface of the lungs, including the fissures between the lobes. It is thin, transparent, and firmly adherent to the lung tissue.
Parietal Pleura
This layer lines the inner surface of the thoracic cavity. It is subdivided based on the region it lines:
- Cervical Pleura (Cupola): Extends superiorly into the neck, covering the apex of the lung.
- Costal Pleura: Lines the inner surface of the ribs and intercostal muscles.
- Mediastinal Pleura: Covers the lateral aspect of the mediastinum.
- Diaphragmatic Pleura: Covers the superior surface of the diaphragm.
B. The Pleural Cavity
This is the potential space between the visceral and parietal pleura. It normally contains only a thin film of serous pleural fluid.
Functions of Pleural Fluid:
- Lubrication: Allows the pleural layers to slide smoothly over each other during breathing, reducing friction.
- Surface Tension: Creates a cohesive force that adheres the lung surface (visceral pleura) to the chest wall (parietal pleura), ensuring the lungs expand and contract with the movements of the thorax.
C. Pleural Recesses (Sinuses)
These are areas where the parietal pleura extends beyond the borders of the lungs, forming potential spaces where fluid can accumulate. They are important clinically.
- Costodiaphragmatic Recess: The largest and most significant recess, located between the ribs and the diaphragm. It is the lowest point of the pleural cavity when upright, making it a common site for fluid accumulation (pleural effusion).
- Costomediastinal Recess: Smaller recesses located anteriorly between the ribs and the mediastinum.
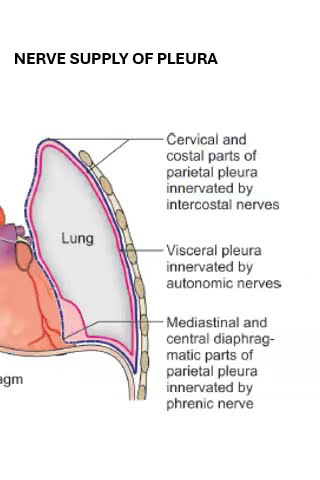
D. Nerve Supply of the Pleura
The nerve supply differs significantly between the two pleural layers, which has major clinical implications for pain sensation.
Parietal Pleura
- Innervation: Somatic sensory nerves.
- Sensitivity: Highly sensitive to pain, touch, temperature, and pressure.
- Nerves:
- Intercostal nerves (for costal pleura).
- Phrenic nerves (for mediastinal and central diaphragmatic pleura).
- Clinical Significance: Inflammation (pleurisy) causes sharp, well-localized pain. Pain from the diaphragmatic pleura can be famously referred to the shoulder tip (via the phrenic nerve).
Visceral Pleura
- Innervation: Autonomic nerves from the pulmonary plexus.
- Sensitivity: Insensitive to pain, touch, and temperature. It does contain stretch receptors.
- Nerves:
- Vagus nerve (parasympathetic).
- Sympathetic trunks.
- Clinical Significance: Lung tissue and the visceral pleura can be extensively diseased without causing pain, until the process affects the pain-sensitive parietal pleura.
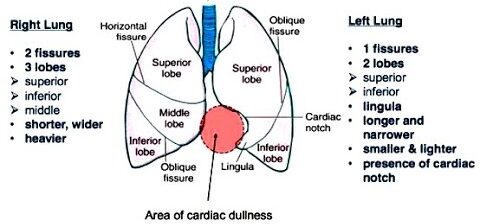
Differences Between Right and Left Lungs
While both lungs perform the same vital function of gas exchange, they exhibit distinct anatomical differences, primarily due to the asymmetrical placement of the heart and great vessels within the thoracic cavity.
A. General Characteristics at a Glance
| Feature | Right Lung | Left Lung |
|---|---|---|
| Size & Weight | Larger and heavier | Smaller and lighter |
| Lobes | 3 Lobes (Superior, Middle, Inferior) | 2 Lobes (Superior, Inferior) |
| Fissures | 2 Fissures (Oblique, Horizontal) | 1 Fissure (Oblique) |
| Cardiac Notch | Absent | Prominent indentation for the heart |
| Lingula | Absent | Present (tongue-like part of superior lobe) |
| Main Bronchus | Shorter, wider, more vertical | Longer, narrower, more horizontal |
B. Detailed Anatomical Differences
1. Lobes and Fissures
The right lung is divided into three lobes by two fissures, while the left lung has only two lobes and one fissure.
Right Lung
- Horizontal Fissure: Separates the superior and middle lobes.
- Oblique Fissure: Separates the middle and inferior lobes.
Left Lung
- Oblique Fissure: Separates the superior and inferior lobes.
- No horizontal fissure.
2. Cardiac Structures and Impressions
The left lung is significantly molded by the heart, creating unique features not seen on the right.
Right Lung
Has a less pronounced cardiac impression and features grooves for the Superior Vena Cava, Azygos vein, and Esophagus.
Left Lung
Features a deep Cardiac Notch and a tongue-like Lingula. It has prominent grooves for the Aortic Arch and the Descending Aorta.
3. Hilum (Root of the Lung)
The arrangement of the bronchus, pulmonary artery, and pulmonary veins differs at the hilum of each lung.
Right Lung Hilum
The bronchus is typically superior and posterior, while the pulmonary artery is anterior to it. The azygos vein arches over the top.
Left Lung Hilum
The pulmonary artery is typically the most superior structure. The bronchus lies posterior and inferior to the artery. The aortic arch passes over the top.
4. Bronchial Tree
The structure of the main bronchi is a key difference with significant clinical implications.
Right Main Bronchus
Shorter, wider, and more vertical.
Left Main Bronchus
Longer, narrower, and more horizontal.
Complications and Common Disorders
The respiratory system is susceptible to a wide range of complications and disorders, affecting any part of the tract from the upper airways to the deep lung parenchyma.
A. Obstructive Lung Diseases
Characterized by increased resistance to airflow, making it difficult to fully exhale.
Chronic Obstructive Pulmonary Disease (COPD)
A progressive disease including Chronic Bronchitis (inflamed, narrow airways with excess mucus) and Emphysema (damaged, inelastic alveoli leading to air trapping). Primarily caused by smoking.
Asthma
A chronic inflammatory disease with reversible airway obstruction, characterized by hyper-responsiveness to triggers leading to wheezing, shortness of breath, and coughing.
Cystic Fibrosis (CF)
A genetic disorder causing thick, sticky mucus that clogs airways, leading to chronic infections and severe lung damage (bronchiectasis).
B. Restrictive Lung Diseases
Characterized by reduced lung volumes and decreased lung compliance (stiffness), making it difficult to fully inhale.
Pulmonary Fibrosis
Scarring and thickening of lung tissue, making the lungs stiff. Can be idiopathic or caused by toxins or autoimmune diseases.
Pneumoconiosis
A group of diseases caused by inhalation of inorganic dusts (e.g., asbestosis, silicosis), leading to inflammation and fibrosis.
Chest Wall & Neuromuscular Disorders
Conditions like scoliosis or diseases like ALS and muscular dystrophy that weaken respiratory muscles or restrict chest movement.
C. Infections of the Respiratory System
Pneumonia
Inflammation of the lung parenchyma where alveoli fill with fluid, impairing gas exchange. Can be caused by bacteria, viruses, or fungi.
Tuberculosis (TB)
A bacterial infection (Mycobacterium tuberculosis) that primarily affects the lungs, causing chronic cough, fever, and night sweats.
D. Vascular Disorders
Pulmonary Embolism (PE)
A life-threatening blockage in a pulmonary artery, typically from a blood clot that traveled from the deep veins of the legs. Causes sudden shortness of breath and sharp chest pain.
Pulmonary Hypertension
High blood pressure in the arteries of the lungs, making it harder for the right side of the heart to pump blood, which can lead to heart failure.
E. Other Significant Disorders
Lung Cancer
Uncontrolled growth of abnormal cells in the lungs. Primarily caused by smoking.
Pneumothorax
A collapsed lung, where air leaks into the pleural cavity, causing the lung to pull away from the chest wall.
Pleural Effusion
An accumulation of excess fluid in the pleural cavity, often caused by heart failure, infections, or cancer.
F. Complications Associated with Respiratory Disorders
Respiratory Failure
The inability of the system to maintain adequate gas exchange, leading to hypoxemia (low blood O₂) and/or hypercapnia (high blood CO₂).
Acute Respiratory Distress Syndrome (ARDS)
A severe, life-threatening lung condition that prevents enough oxygen from getting into the blood, often a complication of other severe illnesses.
Developmental Anomalies of the Respiratory System
Developmental anomalies, also known as congenital anomalies or birth defects, are structural or functional abnormalities that occur during fetal development. Errors during the complex formation of the respiratory tract can lead to a variety of conditions.
A. Anomalies of the Trachea and Bronchi
Tracheoesophageal Fistula (TEF) & Esophageal Atresia (EA)
Description: An abnormal connection between the trachea and esophagus (TEF), often with the esophagus ending in a blind pouch (EA).
Clinical Presentation: Neonates present with choking, coughing, and cyanosis during feeds; inability to pass a nasogastric tube.
Tracheal Stenosis/Atresia
Description: A narrowing (stenosis) or complete absence (atresia) of a segment of the trachea, leading to severe respiratory distress or stridor at birth.
Tracheomalacia/Bronchomalacia
Description: Weakness of the tracheal or bronchial cartilage, leading to airway collapse during exhalation. Causes a barking cough and stridor that worsens with crying.
Bronchial Atresia
Description: A blind-ending bronchus that leads to an over-inflated, air-trapping segment of the lung distally. Often asymptomatic but can cause recurrent infections.
B. Anomalies of the Lungs and Lung Development
Pulmonary Agenesis/Aplasia/Hypoplasia
A spectrum from complete absence of a lung (agenesis) to underdevelopment with reduced size and number of alveoli (hypoplasia). Often associated with conditions that restrict lung growth, like a diaphragmatic hernia.
Congenital Pulmonary Airway Malformation (CPAM)
A non-cancerous lesion of abnormal, cystic lung tissue. Can cause respiratory distress in neonates or lead to recurrent infections in older children.
Bronchopulmonary Sequestration
A mass of non-functional lung tissue not connected to the normal bronchial tree, which receives its blood supply from a systemic artery (like the aorta).
Congenital Lobar Emphysema (CLE)
Over-inflation of a lung lobe due to a "check-valve" mechanism where air gets trapped. Can cause progressive respiratory distress and shift mediastinal structures.
Congenital Diaphragmatic Hernia (CDH)
A defect in the diaphragm allowing abdominal organs to herniate into the chest, leading to severe pulmonary hypoplasia and hypertension. A surgical emergency.
10 Key Developmental Anomalies: A Summary
- Tracheoesophageal Fistula (TEF) & Esophageal Atresia (EA)
- Laryngeal Cleft
- Tracheal Stenosis/Atresia
- Tracheomalacia/Bronchomalacia
- Bronchial Atresia
- Pulmonary Agenesis/Aplasia/Hypoplasia
- Congenital Pulmonary Airway Malformation (CPAM)
- Bronchopulmonary Sequestration
- Congenital Lobar Emphysema (CLE)
- Congenital Diaphragmatic Hernia (CDH)
Test Your Knowledge
Check your understanding of the Respiratory System's development and function.
1. Which of the following is the primary function of the respiratory system?
- Digestion of nutrients
- Regulation of body temperature
- Gas exchange (oxygen and carbon dioxide)
- Blood filtration
2. During fetal development, the respiratory system originates from which germ layer?
- Ectoderm
- Mesoderm
- Endoderm
- Neuroectoderm
3. The production of surfactant, crucial for preventing alveolar collapse, begins to significantly increase during which stage of lung maturation?
- Pseudoglandular stage
- Canalicular stage
- Saccular stage
- Alveolar stage
4. Respiratory Distress Syndrome (RDS) in newborns is primarily caused by:
- Bacterial infection
- Incomplete development of the diaphragm
- Insufficient production of pulmonary surfactant
- Structural abnormalities of the trachea
5. Which of the following describes the condition where the trachea fails to properly separate from the esophagus during development?
- Bronchial atresia
- Tracheoesophageal fistula
- Congenital diaphragmatic hernia
- Pulmonary hypoplasia
6. Which part of the respiratory system is responsible for warming, humidifying, and filtering inhaled air?
- Alveoli
- Bronchioles
- Upper respiratory tract (nasal cavity, pharynx, larynx)
- Diaphragm
7. A congenital diaphragmatic hernia (CDH) is characterized by:
- An abnormal opening in the chest wall.
- A portion of the diaphragm being underdeveloped, allowing abdominal contents to enter the chest cavity.
- Complete absence of lung tissue.
- Narrowing of the bronchi.
8. During the canalicular stage of lung development, what significant event occurs?
- The formation of the laryngotracheal bud.
- The branching of the bronchi and bronchioles is complete.
- The respiratory bronchioles and alveolar ducts begin to form, and vascularization increases.
- Mature alveoli with thin walls are established.
9. Which disorder is characterized by chronic inflammation and narrowing of the airways, often triggered by allergens or irritants?
- Emphysema
- Cystic Fibrosis
- Asthma
- Bronchitis
10. The main muscle responsible for normal, quiet inspiration is the:
- External intercostals
- Internal intercostals
- Diaphragm
- Abdominal muscles
11. The smallest conducting airways in the lungs are called _____________.
12. The final stage of lung maturation, where mature alveoli with thin walls and close contact with capillaries are formed, is known as the _____________ stage.
13. A genetic disorder that causes thick, sticky mucus to build up in the lungs and other organs is _____________.
14. The vocal cords are located within the _____________.
15. _____________ is a condition where the lungs are incompletely developed or abnormally small.
Quiz Complete!
Your Score:
0%
0 / 0 correct